Chapter Nine: Trauma-Informed Care
Overview
Trauma is pervasive throughout society, and community-based services play a vital role in creating trauma-informed responses and environments. Key steps include meeting individuals in a safe, collaborative, and compassionate manner; preventing practices that retraumatize individuals who are seeking help or services; recognizing strengths and the resilience of individuals within their environment and community; and fostering trauma-informed principles in all aspects of the care delivery process.
Learning Objectives
- Understand the principles of trauma-informed care in community health
- Identify the range of symptoms associated with complex trauma and its impact on overall health
- Describe grounding techniques
- Analyze various approaches for trauma management
- Identify things and events that can be sources of trauma
- Recognize the impact of trauma on communities
Key Terms
- trauma
- retraumatization
Content for this chapter was adapted from “Trauma-Informed Care in Behavioral Health Services,” Treatment Improvement Protocol (TIP) Series 57 publication, by the Substance Abuse and Mental Health Services Administration (2014).
Introduction
Trauma-informed care cannot be discussed without mentioning social justice. In fact, trauma-informed care is social justice. Imagine someone who is visiting a community clinic complaining of genital discharge. The patient is asked to undress and wait in the room for the health provider. The patient waits for 5 minutes and then starts screaming that they need to be seen. When the community health nurse enters the room to speak to the patient, the patient states that they need to leave now. They cannot wait any longer. The nurse speaks to the patient and discovers that the patient was raped years ago, and this experience is bringing back all those memories. The nurse then realizes they should have completed a trauma assessment before asking the patient to undress. The nurse then speaks with the patient and uses some of the grounding techniques learned in this chapter to get the patient to stay and be seen. A Healthy People 2030 goal is to increase access to high-quality comprehensive health care services (Office of Disease Prevention and Health Promotion, 2022). Providing every patient with trauma-informed care is a step toward achieving this goal.
Trauma
According to the Trauma and Justice Strategic Initiative put forth by the Substance Abuse and Mental Health Services Administration, “Trauma results from an event, series of events, or set of circumstances that is experienced by an individual as physically or emotionally harmful or threatening and that has lasting adverse effects on the individual’s functioning and physical, social, emotional, or spiritual well-being” (Menschner & Maul, 2016, p. 2). Trauma can affect people of every race, ethnicity, age, sexual orientation, gender, psychosocial background, and geographic region. Trauma can occur at any age or developmental stage, and often, events that occur outside expected life stages are perceived as traumatic (e.g., a child dying before a parent, cancer as a teen, personal illness, job loss before retirement).
It is not just the event itself that determines whether something is traumatic but also the individual’s experience of the event.
A traumatic experience can be a single event, a series of events, and/or a chronic condition (e.g., childhood neglect, domestic violence). Traumas can affect individuals, families, groups, communities, specific cultures, and generations. Trauma overwhelms an individual’s or community’s resources to cope, and it often ignites the “fight, flight, or freeze’’ reaction at the time of the event(s). It frequently produces a sense of fear, vulnerability, and helplessness. Often, traumatic events are unexpected. Individuals may experience the traumatic event directly, witness an event, feel threatened, or hear about an event that affects someone they know. Events may be human made, such as a mechanical error that causes a disaster, war, terrorism, sexual abuse, or violence, or they can be the products of nature (e.g., flooding, hurricanes, tornadoes).
Two people may be exposed to the same event or series of events but experience and interpret these events in vastly different ways. Various biopsychosocial factors influence an individual’s immediate response and long-term reactions to trauma. For most, regardless of the severity of the trauma, the immediate or enduring effects of trauma are met with resilience—the ability to rise above the circumstances or to meet the challenges with fortitude. For some people, reactions to a traumatic event are temporary, whereas others have prolonged reactions that move from acute symptoms to more severe, prolonged, or enduring mental health consequences (e.g., posttraumatic stress and other anxiety disorders, substance use, mood disorders) and medical problems (e.g., arthritis, headaches, chronic pain). Others do not meet established criteria for posttraumatic stress or other mental disorders but encounter significant trauma-related symptoms or culturally expressed symptoms of trauma (e.g., somatization, in which psychological stress is expressed through physical concerns). For that reason, even if an individual does not meet the diagnostic criteria for trauma-related disorders, it is important to recognize that trauma may still affect their lives in significant ways.
Sources and Types of Trauma
The following section reviews various forms and types of trauma in no particular order. It does not cover every conceivable trauma that an individual, group, or community may encounter. The intent is to give nurses working in the community setting a broad perspective of the various categories and types of trauma. The classification of trauma as natural or caused by humans can significantly influence how people react to it and what types of assistance are mobilized in its aftermath. See Table 9.1 for a longer listing of trauma examples.
|
Trauma Caused Naturally |
Trauma Caused by People |
|
|---|---|---|
|
Accidents, Technological Catastrophes |
Intentional Acts |
|
|
Tornado Lightning strike Wildfire Avalanche Physical ailment or disease Fallen tree Earthquake Dust storm Volcanic eruption Blizzard Hurricane Cyclone Typhoon Meteorite Flood Tsunami Epidemic Famine Landslide or fallen boulder |
Train derailment Roofing fall Structural collapse Mountaineering accident Aircraft crash Car accident or malfunction Mine collapse or fire Radiation leak Crane collapse Gas explosion Electrolocation Machinery-related accident Oil spill Maritime accident Accidental gun shooting Sports-related death |
Arson Terrorism Sexual assault and abuse Homicides or suicides Mob violence or rioting Physical abuse and neglect Stabbing or shooting Warfare Domestic violence Poisoned water supply Human trafficking School violence Torture Home invasion Bank robbery Genocide Medical or food tampering |
Trauma from Natural Causes
Natural traumatic experiences can directly affect a small number of people, such as a tree falling on a car during a rainstorm, or many people and communities, as with a hurricane. Natural events, often referred to as “acts of God,” are typically unavoidable. Human-caused traumas are caused by human failure (e.g., technological catastrophes, accidents, malevolence) or by human design (e.g., war). Although multiple factors contribute to the severity of a natural or human-caused trauma, traumas perceived as intentionally harmful often make the event more traumatic for people and communities. How survivors of natural trauma respond to the experience often depends on the degree of devastation, the extent of individual and community losses, and the amount of time it takes to reestablish daily routines, activities, and services (such as returning to school or work, being able to do laundry, having products to buy in a local store).
The amount, accessibility, and duration of relief services can significantly influence the duration of traumatic stress reactions and recovery. Alongside the disruption of daily routines, the presence of community members or outsiders in affected areas may add significant stress or create traumatic experiences in and of themselves. It is not just the natural disaster or event that can challenge an individual or community; often, the event’s consequences and behavioral responses from others within and outside the community push survivors away from effective coping or toward resilience and recovery.
Trauma Caused by Humans
Human-caused traumas are fundamentally different from natural disasters. They are either intentional, such as a convenience store robbery at gunpoint, or unintentional, such as the technological accident of a bridge collapse that occurred in Pittsburgh, Pennsylvania, on January 28, 2022 (Puskar & Scolforo, 2022). The subsequent reactions to these traumas often depend on their intentionality. However, a person or group of people is typically the target of anger and blame from survivors. Survivors of an unintentionally human-caused traumatic event may feel angry and frustrated because of the lack of protection or care offered by the responsible party or government, particularly if there has been a perceived act of omission. After intentional human-caused acts, survivors often struggle to understand the motives for performing the act, the calculated or random nature of the act, and the psychological makeup of the perpetrator(s).
Trauma Affecting Communities and Cultures
Trauma that affects communities and cultures covers a broad range of violence and atrocities that erode the sense of safety within a given community, including neighborhoods, schools, towns, and reservations. These may involve violence in the form of physical or sexual assaults, hate crimes, robberies, workplace or gang-related violence, threats, shootings, or stabbings—for example, the school shooting at Virginia Polytechnic Institute and State University in 2007. They also include actions that attempt to dismantle systemic cultural practices, resources, and identities, such as making boarding school attendance mandatory for Native American children or placing them in non-Native foster homes. Cultural and/or community-based trauma can also occur via indifference or limited responsiveness to specific communities or cultures that are facing a potential catastrophe. Cultural traumas are events that, whether intentionally or not, erode the heritage of culture—as with prejudice, disenfranchisement, and health inequities (e.g., late prenatal care, inability to afford medications, limited access to culturally appropriate health education, vicinity, and quality of affordable medical services), among other examples.
Characteristics of Trauma
Objective Characteristics of Trauma
Trauma can involve a single event, numerous or repeated events, or sustained/chronic experiences. A single trauma is limited to a single point in time. A rape, an automobile accident, or the sudden death of a loved one, these are examples of a single trauma. Some people who experience a single trauma recover without any specific intervention. But for others—especially those with histories of previous trauma or mental or substance use disorders, or those for whom the trauma experience is particularly horrific or overwhelming—a single trauma can result in traumatic stress symptoms and trauma- and stress-related disorders. Single traumas do not necessarily have a lesser psychological impact than repeated traumas.
Some repeated traumas are sustained or chronic. Sustained trauma experiences tend to wear down resilience and the ability to adapt. Some examples include children who endure ongoing sexual abuse, physical neglect, or emotional abuse; people who are in violent relationships; and people who live in chronic poverty. Individuals in chronically stressful, traumatizing environments are particularly susceptible to traumatic stress reactions, substance use, and mental disorders.
Bidirectional relationships exist between trauma and substance use as well as trauma and mental illness. For example, abuse of alcohol and drugs increases the risk of a traumatic experience and creates greater vulnerability to the effects of trauma; substance use reduces a person’s ability to take corrective and remedial actions that might reduce the impact of the trauma. Likewise, traumatic stress leads to a greater likelihood of substance use that, in turn, increases the risk of additional exposure to trauma. Paralleling this bidirectional relationship, mental illness increases vulnerability to the effects of trauma and raises the risk of substance use disorders and additional traumatic events. So too, early exposure to ACEs (adverse childhood experiences) is associated with traumatic stress reactions and subsequent exposure to trauma in adult years.
Subjective Characteristics of Trauma
An important clinical issue in understanding the impact of trauma is the meaning that the survivor has attached to the traumatic experience. Survivors’ unique cognitive interpretations of an event—their beliefs and assumptions—contribute to how they process, react to, cope with, and recover from the trauma. Does the event represent retribution for past deeds committed by the individual or their family? How does the individual attach meaning to their survival? Do they believe it signifies a greater purpose not yet revealed?
People interpret traumatic events in vastly different ways, and many variables shape how an individual assigns meaning to the experience (framing the meaning through culture, family beliefs, prior life experiences and learning, personality and other psychological features, etc.). Even in an event that happens in a household, each family member may interpret the experience differently. Likewise, the same type of event can occur at two different times in a person’s life, but the person’s interpretation of the events may differ considerably because of developmental differences acquired between events, current cognitive and emotional processing skills, availability of and access to environmental resources, and so forth.
Individual Factors
Several factors influence one’s ability to deal with trauma effectively and increase one’s risk for traumatic stress reactions. Individual factors pertain to the individual’s genetic, biological, and psychological makeup and history because they influence the person’s experience, interpretation, and reactions to trauma. However, many factors, not just individual characteristics, influence individual responses to trauma. Failing to recognize that multiple factors, aside from individual attributes and history, influence experiences during and after trauma can lead to blaming the victim for having traumatic stress.
Cultural Meanings of Trauma
It is critical that nurses do not presume to understand the meaning of a traumatic experience without considering the client’s cultural context. Culture strongly influences the perceptions of trauma. Similarly, the sudden death of a family member or loved one can be less traumatic in a culture with a strong belief in a positive afterlife. Nurses need to recognize that their perceptions of a specific trauma could differ from those of their clients. Be careful not to judge a client’s beliefs in light of your own value system.
Understanding the Impact of Trauma
Trauma-informed care involves a broad understanding of traumatic stress reactions and common responses to trauma. Nurses need to understand how trauma can affect treatment presentation, engagement, and the outcome of health services. Trauma affects everyone differently, including one-time, multiple, or long-lasting repetitive events. Some individuals may display criteria associated with posttraumatic stress disorder (PTSD), but many more individuals will exhibit resilient responses or brief subclinical symptoms or consequences that fall outside of diagnostic criteria. The impact of trauma can be subtle, insidious, or outright destructive. How an event affects an individual depends on many factors, including individual characteristics, the type and characteristics of the event(s), developmental processes, the meaning of the trauma, and sociocultural factors.
Trauma Reactions
A variety of reactions are often reported and/or observed after trauma. Most survivors exhibit immediate reactions, yet these typically resolve without severe long-term consequences. This is because most trauma survivors are highly resilient and develop appropriate coping strategies, including the use of social support, to deal with the aftermath and effects of trauma. Most recover with time, show minimal distress, and function effectively across major life areas and developmental stages. Even so, clients who show little impairment may still have subclinical symptoms or symptoms that do not fit the diagnostic criteria for acute stress disorder (ASD) or PTSD. Only a small percentage of people with a history of trauma show impairment and symptoms that meet the criteria for trauma-related stress disorders, including mood and anxiety disorders. See Table 9.2 for common responses to trauma.
|
Immediate Reactions to Trauma |
Delayed Reactions to Trauma |
|
|---|---|---|
|
Emotional |
|
|
|
Physical |
|
|
|
Cognitive |
|
|
|
Behavioral |
|
|
|
Existential |
|
|
Trauma-Informed Care
Screening and Assessment
Screening
Screening begins by determining whether the person has a history of trauma and whether the person has trauma-related symptoms. Screening obtains answers to “yes” or “no” questions: “Has this client experienced a trauma in the past?” and “Does this client at this time warrant further assessment regarding trauma-related symptoms?” If someone acknowledges a trauma history, then further screening is necessary to determine whether trauma-related symptoms are present. However, the presence of such symptoms does not necessarily say anything about their severity, nor does a positive screen indicate that a disorder exists. Positive screens indicate only that assessment or further evaluation is warranted, and negative screens do not necessarily mean that an individual does not have symptoms that warrant intervention.
Screening procedures should always define the steps to take after a positive or negative screening. That is, the screening process establishes precisely how to score responses to screening tools or questions and clearly defines what constitutes a positive score (called a “cutoff score”) for a particular potential problem. The screening procedures detail the actions to take after a client scores in the positive range. Clinical supervision is helpful—and sometimes necessary—in judging how to proceed. Trauma-informed screening is essential to the intake evaluation and treatment planning process, but it is not an end in itself. Screening processes can be developed that allow staff without advanced degrees or graduate-level training to conduct them, whereas assessments for trauma-related disorders require a mental health professional trained in assessment and evaluation processes.
The most important domains to screen among individuals with trauma histories include these:
- Trauma-related symptoms
- Depressive or dissociative symptoms, sleep disturbances, and intrusive experiences
- Past and present mental disorders, including typically trauma-related disorders (e.g., mood disorders)
- Severity or characteristics of a specific trauma type (e.g., forms of interpersonal violence, adverse childhood events, combat experiences)
- Substance use
- Social support and coping styles
- Availability of resources
- Risks for self-harm, suicide, and violence
- Health screenings
Assessment
When a client has substance use disorder, trauma-related symptoms, or mental disorders, the agency or counselor should follow up with an assessment. A positive screening calls for more action—an assessment that determines and defines presenting struggles to develop an appropriate treatment plan and to make an informed and collaborative decision about treatment placement. The assessment determines the nature and extent of the client’s problems; it might require the client to respond to written questions, or it could involve a clinical interview by mental health or substance use professionals qualified to assess the client and arrive at a diagnosis. A clinical assessment delves into a client’s past and current experiences, psychosocial and cultural history, and assets and resources. Assessment protocols can require more than a single session to complete and should also use multiple avenues to obtain the necessary clinical information, including self-assessment tools, past and present clinical and medical records, structured clinical interviews, assessment measures, and collateral information from significant others, other health professionals, and agencies.
Qualifications for conducting assessments and clinical interviews are more rigorous than for screening. Advanced degrees, licensing or certification, and special training in administration, scoring, and interpretation of specific assessment instruments and interviews are often required. For people with histories of traumatic life events who screen positive for possible trauma-related symptoms and disorders, a thorough assessment gathers all relevant information necessary to understand the role of the trauma in their lives; appropriate treatment objectives, goals, planning, and placement; and any ongoing diagnostic and treatment considerations, including reevaluation or follow-up. Overall, the assessment may indicate symptoms that meet diagnostic criteria for a substance use or mental disorder or a milder form of symptomatology that does not reach a diagnostic level, or it may reveal that the positive screen was false and that there is no significant cause for concern.
Information from an assessment is used to plan the client’s treatment. The plan can include such domains as a level of care, acute safety needs, diagnosis, disability, strengths and skills, support network, and cultural context. Assessments should recur throughout treatment. Ongoing assessment during treatment can provide valuable information by revealing further details of trauma history as clients’ trust in staff members grows and by gauging clients’ progress.
Strategies for Screening and Assessments
The success of treatment can be enhanced by paying careful attention to the approach to the screening and assessment process by using the following strategies:
- Clarify to the client what to expect in the screening and assessment process
- Approach the client in a matter-of-fact and supportive manner
- Respect the client’s personal space
- Adjust tone and speech volume to suit the client’s level of engagement and comfort in the interview process
- Provide culturally appropriate symbols of safety in the physical environment
- Be aware of one’s own emotional responses to hearing clients’ trauma histories
- Overcome linguistic barriers via an interpreter
- Elicit only the information necessary for determining a history of trauma and the possible existence and extent of traumatic stress symptoms and related disorders
- Use self-administered, written checklists rather than interviews (when possible) to assess trauma
- Interview the client if they have trouble reading or writing or cannot complete a checklist
- Allow time for the client to become calm and oriented to the present if the client has very intense emotional responses when recalling or acknowledging a trauma
- Avoid phrases that imply a judgment about the trauma
- Provide feedback about the results of the screening
- Be aware of the possible legal implications of assessment
Barriers to Screening and Assessment
Without screening, it is not necessarily easy or obvious to identify an individual who has survived trauma. Moreover, some clients may deny that they have encountered trauma and its effects even after being screened or asked direct questions to identify the occurrence of traumatic events.
The two main barriers to evaluating trauma and its related disorders in health care settings are clients not reporting trauma and nurses and other health care providers overlooking trauma and its effects. Concerning the first main barrier, some events affect the person’s responses to them and the meanings they attach to the event. Certain situations make it more likely the event will be experienced as traumatic by one person but considered nontraumatic by another. A history of trauma encompasses the experience of a potentially traumatic event and the likelihood that the client will not be forthcoming about traumatic events or their responses to those events. Some clients might not have ever thought of a particular event or their response to it as traumatic and thus might not report or even recall the event. Some clients might be reluctant to discuss something that they sense might bring up uncomfortable feelings (especially with a counselor they have met only recently). Clients may avoid openly discussing traumatic events or have difficulty recognizing or articulating their experience of trauma for other reasons, such as feelings of shame, guilt, or fear of retribution by others associated with the event (e.g., in cases of interpersonal or domestic violence). Others may deny their history because they are tired of being interviewed or asked to fill out forms and may believe it does not matter anyway.
Managing Trauma
Grounding Techniques
Grounding techniques are important skills for assessors and all other behavioral health service providers who interact with traumatized clients (e.g., nurses, security, administrators, clinicians). Even if you do not directly conduct therapy, knowledge of grounding can help defuse an escalating situation or calm a client who is triggered by the assessment process. Grounding strategies help a person who is overwhelmed by memories or strong emotions or is dissociating; they help the person become aware of the here and now. A useful metaphor is an experience of walking out of a movie theater. When the person dissociates or has a flashback, it’s like watching a mental movie; grounding techniques help the person step out of the movie theater into the daylight and the present environment. The client’s task is not only to hold on to moments from the past but also to acknowledge that what they were experiencing is from the past. Try the following techniques (Melnick & Bassuk, 2000):
- Ask the client to state what they observe.
Guide the client through this exercise by using statements like these: “You seem to feel very scared/angry right now. You’re probably feeling things related to what happened in the past. Now, you’re in a safe situation. Let’s try to stay in the present. Take a slow deep breath, relax your shoulders, and put your feet on the floor; let’s talk about what day and time it is, notice what’s on the wall, … What else can you do to feel okay in your body right now?”
- Help the client decrease the intensity of the effect.
“Emotion dial”: A client imagines turning down the volume on their emotions. Clenching fists can move the energy of emotion into fists, which the client can then release. Guided imagery can be used to visualize a safe place.
Distraction (see Item 3, next). Use strengths-based questions (e.g., “How did you survive?” or “What strengths did you possess to survive the trauma?”).
- Distract the client from unbearable emotional states.
Have the client focus on the external environment (e.g., naming red objects in the room).
Ask the client to focus on recent and future events (e.g., “to do” list for the day). Help the client use self-talk to remind themself of current safety. Use distractions, such as counting, to return the focus to current reality. Somatosensory techniques (e.g., toe-wiggling, touching a chair) can remind clients of current reality.
- Ask the client to use breathing techniques.
Ask the client to inhale through the nose and exhale through the mouth. Have the client place their hands on their abdomen and then watch the hands go up and down while the belly expands and contracts.
Psychoeducation
Trauma-informed education informs clients about traumatic stress and trauma-related symptoms and disorders and the consequences of trauma exposure. It focuses on giving information to clients to help normalize presenting symptoms, highlighting potential short- and long-term consequences of trauma and various paths to recovery, and underscoring the message that recovery is possible. Education frequently takes place before or immediately following an initial screening as a way to prepare clients for hearing results or to place the screening and subsequent assessment findings in the proper context.
However, education does not necessarily constitute a stand-alone treatment; rather, it can be conceptualized as a first step and/or component of a more comprehensive treatment. Nonetheless, education may be a prevention and intervention strategy for individuals with histories of trauma without current consequences or symptoms and/or those who have reported a resolution of past trauma(s). For example, some clients may have significantly delayed onset of traumatic stress symptoms. In this scenario, earlier education can enhance the recognition of symptoms and ease the path to seeking treatment. Some clients do not recognize the link between their current difficulties and their trauma histories; education can help them understand the possible origin of their difficulties.
Psychoeducation presents trauma-related symptoms that follow a trauma as normal reactions. Identifying the source of clients’ current difficulties and framing them as normal thoughts, emotions, and behaviors in response to trauma helps trauma survivors. Many report a reduction in the intensity of the difficulties or symptoms. Often, a client will express relief that their reactions are normal. The U.S. Department of Veterans Affairs National Center’s PTSD educational handouts on traumatic stress reactions may be useful here. Psychoeducation goes beyond identifying traumatic stress symptoms and/or learning about trauma’s psychological, cognitive, and physical impacts. Numerous curricula are available that use psychoeducation as a first-line or complementary approach to trauma-specific therapies to enhance coping strategies in key areas, including safety, emotional regulation, help-seeking, avoidant behavior, and so forth. An example is S.E.L.F., a trauma-informed psychoeducational group curriculum with educational components related to trauma recovery in the following areas: creating Safety, regulating Emotions, addressing Loss, and redefining the Future (Bloom et al., 2021).
Normalize Symptoms
Symptoms of trauma can become serious barriers to recovery from substance use and mental disorders, including trauma-related ones. Counselors should know how trauma symptoms can present and how to respond to them when they do appear. A significant step in addressing symptoms is normalizing them. People with traumatic stress symptoms need to know that their symptoms are not unique and that their reactions are common to their experience(s). Often, normalizing symptoms gives considerable relief to clients who may have thought that their symptoms signified some pervasive, untreatable mental disorder.
Identify Triggers and Trauma
Many clients who have traumatic stress are caught off guard by intrusive thoughts, feelings, sensations, or environmental cues of the trauma. This experience can be quite disconcerting, but often, the individual does not draw an immediate connection between the internal or external trigger and their reactions. At other times, the trigger is so potent that the individual is unable to discern the present trigger from the past trauma and begins to respond as if the trauma is reoccurring. A key step in identifying triggers is to reflect on the situation, surroundings, or sensations before the strong reaction. This step may enable the connections among these cues, the past trauma(s), and the client’s reaction to be determined. Once the cue is identified, the next step is to discuss how it is connected to past trauma. For some cues, there will be an obvious and immediate connection (e.g., having someone say “I love you” in a significant relationship as an adult and connecting this to an abuser who said the same thing before a sexual assault). Other cues will not be as obvious. With practice, the client can begin to track back through what occurred immediately before an emotional, physical, or behavioral reaction and then examine how that experience reminds them of their past.
Teach Balance
A thin line is walked when addressing trauma. On the one hand, too much work focused on highly distressing content can turn a desensitization process into a session whereby the client dissociates, shuts down, or becomes emotionally overwhelmed. On the other hand, too little focus by the client or counselor can easily reinforce avoidance and confirm the client’s internal belief that it is too dangerous to deal with the aftermath of the trauma.
Several trauma-specific theories offer guidelines on acceptable levels of distress associated with the traumatic content that the therapy addresses. For example, some traditional desensitization processes start at an incredibly low level of subjective distress, gradually working up through a hierarchy of trauma memories and experiences until those experiences produce minimal reactions when paired with some coping strategy, such as relaxation training. Other desensitization processes start at a higher level of intensity to provide more rapid extinction of traumatic associations and to decrease the risk of avoidance—a behavior that reinforces traumatic stress.
Working with trauma is a delicate balancing act between the development and/or use of coping strategies and the need to process the traumatic experiences. Individuals will choose different paths to recovery; it is a myth that every traumatic experience needs to be expressed and every story told. For some individuals, the use of coping skills, support, and spirituality are enough to recover. Regardless of theoretical beliefs, counselors must teach coping strategies as soon as possible. Retraumatization is a risk whenever clients are exposed to their traumatic histories without sufficient tools, support, and safety to manage emotional, behavioral, and physical reactions.
Retraumatization
Retraumatization occurs when clients experience something that makes them feel as though they are undergoing another trauma, as was illustrated in the example at the beginning of this chapter. Unfortunately, treatment settings and clinicians can create retraumatizing experiences, often without being aware of it. Sometimes clients themselves are not consciously aware that a clinical situation has triggered a traumatic stress reaction. Agencies that anticipate the risk for retraumatization and actively work on adjusting program policies and procedures to remain sensitive to the histories and needs of individuals who have undergone past trauma are likely to succeed in providing care, retaining clients, and achieving positive outcomes. A number of staff and agency issues can cause retraumatization:
- Being unaware that the client’s traumatic history significantly affects their life
- Failing to screen for trauma history prior to treatment planning
- Challenging or discounting reports of abuse or other traumatic events
- Using isolation or physical restraints
- Using experiential exercises that humiliate the individual
- Endorsing a confrontational approach in counseling
- Allowing the abusive behavior of one client toward another to continue without intervention
- Labeling behavior and/or feelings as pathological
- Failing to provide adequate security and safety within the program
- Limiting the participation of the client in treatment decisions and planning processes
- Minimizing, discrediting, or ignoring client responses
- Disrupting counselor–client relationships by changing counselors’ schedules and assignments
- Obtaining urine specimens in a nonprivate setting
- Having clients undress in the presence of others
- Inconsistently enforcing rules and allowing chaos in the treatment environment
- Imposing agency policies or rules without exceptions or an opportunity for clients to question them
- Enforcing new restrictions within the program without staff–client communication
- Limiting access to services for ethnically diverse populations
- Accepting agency dysfunction, including lack of consistent, competent leadership
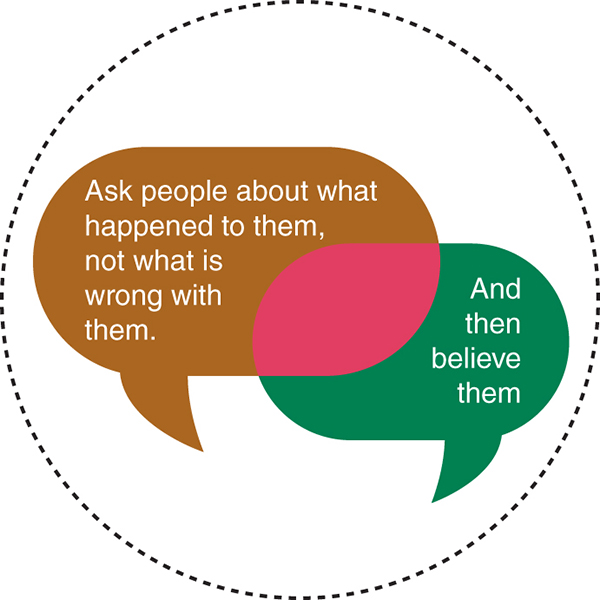
The Nurse’s Role in Trauma-Informed Care
Many individuals who seek care in community settings have histories of trauma, but they often do not recognize the significant effects of trauma in their lives; either they do not draw connections between their trauma histories and their presenting problems or they avoid the topic altogether. Likewise, community health nurses may not ask questions that elicit a client’s history of trauma, may feel unprepared to address trauma-related issues proactively, or may struggle to address traumatic stress effectively within the constraints of their treatment program, the program’s clinical orientation, or their agency’s directives. By recognizing that traumatic experiences tie closely into behavioral health problems, nurses and community-based programs can begin to build a trauma-informed environment across the continuum of care. Key steps include meeting client needs in a safe, collaborative, and compassionate manner; believing what the patient says about their experience; preventing treatment practices that retraumatize people with histories of trauma who are seeking help or receiving services; building on the strengths and resilience of clients in the context of their environments and communities; and endorsing trauma-informed principles in agencies through support, consultation, and supervision of staff.
Practice Application
➔ Setting the Scene
Stressful time often denotes being bombarded with many things at one time, perceived or actual, without sufficient time or ability to address them emotionally, cognitively, spiritually, and/or physically. The same goes for trauma: rapid exposure to numerous traumas one after another lessens one’s ability to process the event before the next onslaught. This creates a cumulative effect, making it more difficult to heal from any singular trauma.
➔ Think About It
Imagine an event that was particularly stressful (but not traumatic) in your life. Revisit this period as an observer watching the events unfold.
- What made this event particularly stressful? Was it difficult to manage one situation before another circumstance came along demanding your time?
- How did you process the event? What were the resources you used? Did you learn anything from processing it?
- Are there any tools you’d use to process similar situations moving forward?
- Suppose in your work area you were exposed to multiple poor patient outcomes over several days.
- How do you think this situation might affect you and your role as a nurse?
- Would you be able to use some of these same resources that you used to process your stressful event? Why or why not?
Additional Resources
ACEs Aware – Trauma-Informed Care
The National Child Traumatic Stress Network – Trauma-Informed Care
Virginia Department of Behavioral Health and Developmental Services – Trauma Informed Care
References
Bloom, S. L., Foderaro, J. F., & Ryan, R. (2021). S.E.L.F.: A trauma-informed psychoeducational group curriculum. U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration. https://sandrabloom.com/wp-content/uploads/FREE-INTRODUCTORY-MATERIALS-WITH-SAMPLE-LESSON-1.pdf
Briere, J., & Scott, C. (2006). Central issues in trauma treatment. In Principles of trauma therapy: A guide to symptoms, evaluation, and treatment (pp. 67–85). Sage Publications.
Foa, E. B., Stein, D. J., & McFarlane, A. C. (2006). Symptomatology and psychopathology of mental health problems after disaster. The Journal of Clinical Psychiatry, 67(Suppl. 2), 15–25.
Melnick, S. M., & Bassuk, E. L. (2000). Identifying and responding to violence among poor and homeless women. National Healthcare for the Homeless Council. https://nhchc.org/wp-content/uploads/2019/08/IdentifyingRespondingtoDomesticViolence_2000.pdf
Menschner, C., & Maul, A. (2016). Key ingredients for successful trauma-informed care implementation (p. 12) [Issue brief]. Center for Health Care Strategies, U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration. https://www.samhsa.gov/sites/default/files/programs_campaigns/childrens_mental_health/atc-whitepaper-040616.pdf
Office of Disease Prevention and Health Promotion. (2022). Healthy People 2030. https://www.health.gov/healthypeople
Pietrzak, R. H., Goldstein, R. B., Southwick, S. M., & Grant, B. F. (2011). Personality disorders associated with full and partial posttraumatic stress disorder in the U.S. population: Results from Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Psychiatric Research, 45(5), 678–686. https://doi.org/10.1016/j.jpsychires.2010.09.013
Puskar, G., & Scolforo, M. (2022). Pittsburgh bridge collapses, drops city bus into ravine. AP NEWS. https://apnews.com/article/joe-biden-business-pittsburgh-bridge-collapses-b91476e4d1dc1c7839bd0c39e7be186e
Substance Abuse and Mental Health Services Administration. (2014). Trauma-informed care in behavioral health services. Treatment Improvement Protocol (TIP) Series 57. U.S. Department of Health and Human Services. Substance Abuse and Mental Health Services Administration. https://www.store.samhsa.gov/sites/default/files/d7/priv/sma14-4816.pdf

