Chapter One: Community and Public Health Policy
Overview
This chapter introduces the learner to the foundations of health policy. Policy shapes our experiences at all levels of society. This chapter focuses on the policy’s structure, impact, and influence on community and population health. In keeping with the aims of this book, the policy will be discussed through the lens of social justice.
Learning Objectives
- Understand the impact of policies on population outcomes, including social justice and health equity
- Summarize the structural components of legal, regulatory, and policy guidelines for the community and public health
- Analyze system-level and public policy influence on the community and public health overall
- Understand how to advance public health policy through various advocacy strategies
- Identify opportunities to influence policy change
Introduction
Community health nurses are strategically positioned to function as change agents in the community. Actively engaging the understanding of the importance of health policy, navigating the current policy landscape, identifying opportunities to contribute their expertise as health care collaborators, and bridging the gaps in needed services offer community health nurses a unique opportunity to help maximize health potential for all citizens within their sphere of influence. Community nurses can apply knowledge of health policy to advocate for individuals, communities, and populations and enable changes that result in community thriving.
Understanding Health Policy
Health policy is the result of a public decision-making process that makes goal-directed health-related processes (Keller & Ridenour, 2021). Most often, health policy is visible in governmental policy and legislative decisions at the local, state, and national levels, although policymaking also happens through corporations, institutional boards, and executives. Nurses are critical in advocating for policies that can affect patients and the profession. Nurse advocacy is particularly important to represent vulnerable populations and those who have been historically underrepresented. Policy advocacy can be especially powerful when the nursing profession speaks with a united voice on issues that affect health outcomes. Nurses can influence health policy by understanding and engaging in the policy process on multiple levels, including interpreting, evaluating, and leading policy change.
Health policy, at its best, is meant to promote the health of individuals, communities, and populations. Policy decisions significantly affect health and well-being, and evidence-based health policies can help prevent disease and promote health. For example, smoke-free policies can prevent smoking initiation and increase smoking cessation attempts. Similarly, policies requiring community water systems to provide fluoridated water can improve oral health.
However, health policy is rarely straightforward and often presents complex legal, ethical, and social questions. From a community health viewpoint, it is the responsibility of the government to create a health policy that protects and promotes the health of individuals and the community and to do so in a manner that respects human rights, including the right to self-determination, privacy, and nondiscrimination. Communities must operate within the context of federal and state policies that can affect local government decisions relevant to health through laws and regulations. Widely recognized policies include those that fund or regulate health care delivery services; but policies in all types of areas, from education to land use and housing, the environment, and criminal justice, can be relevant to health and health care disparities within communities.
At the state and federal levels, formal development of health policy is distributed among the three branches of government: the executive, the legislative, and the judicial. Health policy at these levels addresses many issues, such as health care, public health initiatives, and biotechnology. Examples of health care decisions affected by health care policies include reproductive rights, approaches to mental health care, civil rights of differently abled populations, drug pricing, and access to health care, among others (Gostin, 1995). Policies can vary across geographic areas and populations, providing important opportunities or constituting barriers to promoting health equity (Baciu et al., 2017). Other legislative policies are far-reaching.
The Civil Rights Act of 1964 was a sweeping legislative act signed into law by President Johnson on July 2, 1964. This act prohibited discrimination in public places. It provided for the integration of schools and other public facilities and made employment discrimination illegal. Though this act mandated desegregation, institutions have struggled to adequately represent minorities that reflect the geographical populations (Civil Rights Act, 1964). When it comes to health care, large racial disparities continue to persist. For example, people of color are considerably fewer than Whites in medical and nursing schools (Association of American Medical Colleges, 2021; Campaign for Action, n.d.). Yet, diversity of health care teams is linked to improved health outcomes and culturally competent care (Cohen et al., 2002). We can begin to understand, then, how systematic adherence to policy such as the Civil Rights Act of 1964 can contribute to quality education and college preparation, leading to increasing qualified health care applicants and successful graduation. Nurses can inform themselves and others on how policy can directly and indirectly influence health care accessibility and quality.
Underserved, Vulnerable, and Special Needs Populations
The U.S. Department of Health and Human Services (DHHS) characterizes underserved, vulnerable, and special needs populations as communities that include members of minority populations or individuals who have experienced health disparities. Members of minority populations or individuals who have experienced health disparities include but are not limited to these groups:
- Latino populations
- African American populations
- American Indian/Alaska Native populations
- Refugees
- Individuals with limited English proficiency
- Young adults and postsecondary graduating students who have no health coverage options through a parent’s plan, a student plan, or an employer plan
- New mothers and women with children
- Individuals with disabilities
- Consumers not enrolled in Medicaid coverage despite being eligible
The term vulnerable is often used interchangeably with underserved. Whereas underserved communities have limited access to health care services, vulnerable individuals tend to experience additional barriers to getting care. For example, an individual with limited English proficiency is considered vulnerable but not underserved (e.g., the consumer might have access to high-quality care). However, there can be considerable overlap among vulnerable and underserved populations, with many individuals falling into both categories.
Vulnerable populations include those who share one or more of the following characteristics:
- High risk for multiple health problems and/or preexisting conditions
- Limited life options (e.g., financial, educational, housing)
- Fear and distrust in accessing government programs or disclosing sensitive information about family members
- Limited ability to understand or give informed consent without the assistance of language services (e.g., consumers with limited English proficiency or cognitive impairments)
- Mobility impairments
- No access to transportation services
- Lowered capacity to communicate effectively
- Vulnerability to any type of discrimination
Underserved populations include those who share one or more of the following characteristics:
- Receive fewer health care services
- Encounter barriers to accessing primary health care services (e.g., economic, cultural, and/or linguistic)
- Lack familiarity with the health care delivery system
- Face a shortage of readily available providers
Nursing and Health Policy
The better informed nursing professionals and communities are about the implications of policy changes, the greater their ability to respond, particularly in addressing health disparities and helping achieve change in the determinants of health. Likewise, the more the needs of communities are considered in policy decision-making, the more effective these policies will be (Baciu et al., 2017). The socioeconomic and political drivers in communities and their political context are highlighted in Figure 1.1, inspired by the National Institutes of Health model for ways to promote health equity presented in Communities in Action: Pathways to Health Equity Report. The report provided a conceptual model for community solutions to promote health equity (Baciu et al., 2017). The policy context is highlighted here to convey the focus of this chapter (Baciu et al., 2017).

Health policy legislation often represents the competing values of various stakeholders and interest groups and assessments of available data. Interest groups and stakeholders often consider policy questions through a distinct values lens, including individual interpretations of right and wrong, good and bad, necessary and unnecessary.
A number of critical factors influence effective health care policy development:
- Policymakers should be objective.
- Decision-makers should have no conflict of interest.
- Policymakers should understand the data and the arguments presented.
- Health policies should not seriously burden individual rights to liberty, privacy, and nondiscrimination.
- Decision-making bodies should be positioned to receive and evaluate full and objective information on all aspects of a health policy.
- Policymakers should have well-considered criteria for making the decision.
- Policymakers should pursue a fair process to arrive at the decision.
Criteria for Policy Development
Nursing and community health practitioners can play an active role in supporting the development of criteria that decision-makers can use when they are formulating health policy goals. This support may include establishing the scientific, social, and ethical parameters for decision-making, which may help reduce biases that can undermine health policy development. Among criteria to consider are these:
- Examine the public health interest. Does the proposed policy seek to achieve a compelling health objective? The policymaker should clearly and narrowly define the policy’s health purpose(s). This protects against decision-making biases, helps communities understand the policy rationale, and facilitates public debate.
- Examine the overall effectiveness of the policy. Is the proposed policy likely to be effective in achieving the stated goal(s)? This criterion requires an assessment of whether the policy is an appropriate intervention to achieve the stated objectives and whether it is likely to lead to effective action. The policymaker should gather scientific data and apply logic to analyze whether a policy will be effective.
- Evaluate whether the policy is well targeted. Is the proposed policy narrowly focused on the health problem? A decision-maker should determine whether a policy is narrowly tailored to address the specific health problem or whether it is over- or underinclusive. Overbroad policies target a population that is much larger than necessary to achieve the health objective.
- Identify the human rights burdens. Doing this requires an inquiry into the nature of human rights violations, invasiveness, scope, and duration. Does the policy interfere with the right to liberty, autonomy, privacy, or nondiscrimination? For example, a policy that requires women to use contraceptives as a condition of receiving welfare benefits might interfere with the right to reproductive privacy and discriminate against women (because the policy does not apply to men) and persons who are economically disadvantaged (because the policy does not affect higher income women). It may also burden dependent children’s social and economic rights if benefits are withdrawn.
- Examine whether the policy is the least restrictive alternative. A policymaker should assess whether the health objective could be achieved as well, or better, with fewer restrictions on human rights. This approach helps to ensure that a policymaker considers alternatives that may better accommodate societal and individual interests (Gostin, 1995).
Impacts of Policies on Community Health
It is clear that health policies at the local, state, and federal levels can influence the health of both individuals and the population-at-large. For example, consider the following:
- Increasing taxes on tobacco sales can improve population health by reducing the number of people using tobacco products.
- The Affordable Care Act, implemented in 2010, significantly increased the number of insured Americans.
- The Health Insurance Portability and Accountability Act protects American workers by allowing them to carry health insurance policies from job to job.
- Along with Medicaid, the Children’s Health Insurance Program has created a strong foundation for delivering health coverage to children living in low-income households.
The impact of policies or a lack of policy on non-health domains—economic and environmental domains, for example—can also directly affect community health. Health policies, as well as policies that have an impact on the health of communities, may disproportionately affect vulnerable communities with limited resiliency as a result of socioeconomic barriers. For example, transportation policies, living wage policies, and zoning can dramatically affect health outcomes, particularly in vulnerable communities (Benjamin, 2018; Rieck & Lundin, 2018).
Population Health Outcomes
Researchers, patients, providers, and policymakers have worked to identify, understand, and eliminate the disparities experienced by different racial and ethnic groups across the health care system. In 1985, DHHS published the report of the Secretary’s Task Force on Black and Minority Health (Heckler, 1986), marking the U.S. government’s first comprehensive study of racial and minority health. Since then, DHHS and other stakeholders have continued this work, including throughout the National Healthcare Quality and Disparities Report. The growing evidence base shows that patients of different racial and ethnic groups experience the quality of care inequitably and disparately. For example, although Black, Hispanic, American Indian, and Alaska Native communities have all experienced improvements in health care quality, significant disparities in all domains of health care quality persist. Rates of quality improvement exceeded those White Americans experienced in 11% of all quality measures, but that change has not been enough to eliminate disparities (Agency for Healthcare Research and Quality [AHRQ], 2021).
The National Healthcare Quality and Disparities Report notes that a significant disparity persists despite a decrease in HIV death rates, including in Black populations. “From 2000 to 2018, HIV deaths in Black populations decreased from 23.3 deaths to 6.2 deaths per 100,000 population. Still, deaths in Black populations remain more than six times as high as HIV deaths in White populations (0.9 deaths per 100,000 population)” (AHRQ, 2021).
Additionally, “from 2001 to 2018, the incident rates of end-stage renal disease due to diabetes decreased 48% from 526 to 273.1 events per million population in American Indian/Alaska Native communities and decreased 29% from 525.7 to 372.2 per million population in Black communities. Despite these gains, significant disparities persist among non-Hispanic American Indian and Alaska Native, Black, and White populations, with respective incident rates of 273.1, 372.2, and 152.2 events per million population in 2018” (AHRQ, 2021).
The intersections of these variables, race/ethnicity, socioeconomic status, gender, age, and geography, are complex, and health disparities can be partially, yet directly, linked to health policy. Recommended reading includes the full National Healthcare Quality and Disparities Report (AHRQ, 2021).
Social Justice and Health Equity
Social justice is the view that everyone deserves equal rights and opportunities, including the right to good health (American Public Health Association, 2021). An avoidable inequity resulting from health policy is unjust.
Health disparity and health inequity play a role in fostering social disadvantage and interfere with social justice within a community. The term social disadvantage implies that a person or group of persons are compromised or marginalized because of their position in society. What follows is a limited or restricted opportunity to fully participate in society and, in turn, a limited opportunity to prosper and contribute. Individuals or persons who are socially disadvantaged through the means of social structures, such as policy, are denied the chance to reach and enjoy their full potential and do not experience the same benefits within society as others do. Social disadvantage is not the same as unavoidable physical disadvantage. For example, when people with disabilities are placed at an avoidable disadvantage in society because they lack necessary support (e.g., accessible public buildings and transportation) or are subject to discrimination in hiring, what results is discriminatory treatment, regardless of intention (Braveman et al., 2011). In these examples, the policy might ensure that public buildings are accessible and that equal employment laws can protect individuals from discrimination in hiring.
Social determinants of health (SDOH) are broadly defined by factors such as economic and job stability, education and health care access, social and community context, and neighborhood and built environment (Centers for Disease Control and Prevention, 2021). When individuals are denied opportunities in any of these domains, they may also have limited access to quality health care services and experience greater risk for illness or severity of illness. Impaired health further restricts the opportunity to be fully engaged in society, again intruding on these individuals’ rights to be full participants in their community. This is considered unjust.
Figure 1.2 illustrates that community health nurses must reflect on their values and assumptions. Then they can utilize their practice experience and study evidence-based research to address SDOH elements as shown in the blue column with strategies to undertake in the green column, one of which is a policy with the ultimate goal of health and well-being indicated in red.
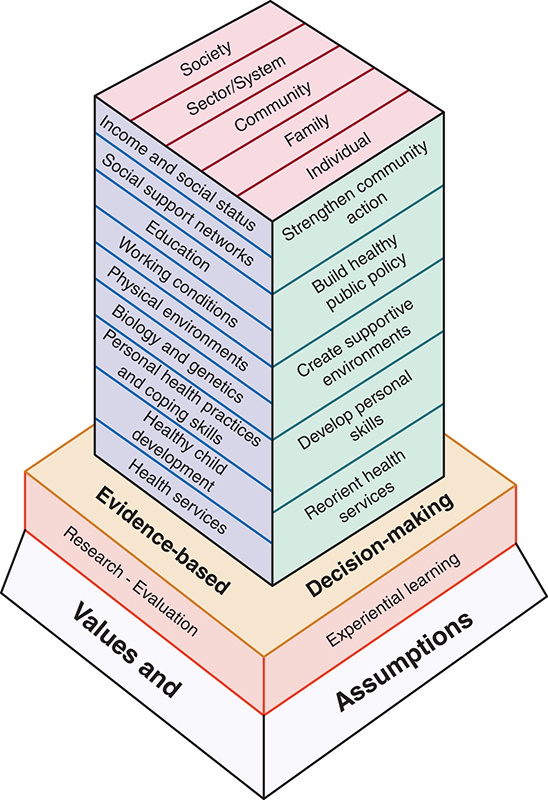
Long Description for Figure 1.2
The base of the diagram represents values and assumptions, with research and evaluation below evidence-based practice, and experiential learning below decision-making. S D O H elements are listed above evidence-based learning. They are as follows. Income and social status, social support networks, education, working conditions, physical environments, biology and genetics, personal health practices and coping skills, healthy child development, and health services. The strategies to address S D O H, are listed above decision-making, as follows. Strengthening community action, building healthy public policy, creating supportive environments, developing personal skills, and reorienting health services. The top block represents society, sector or system, community, family, and individual.
Healthy People 10-Year Plan
The DHHS initiative Healthy People 2030, referred to as the nation’s 10-year plan, sets data-driven national objectives to improve health and well-being and has identified specific objectives aimed at reducing health care disparity and improving the health of vulnerable and underserved populations (Office of Disease Prevention and Health Promotion, n.d.). The plan focuses on the following SDOH aspects and helps drive the nation’s health care policy agenda:
- Economic Stability
In the United States, one in 10 people lives in poverty, with many unable to afford things like healthy foods, health care, and housing. While individuals with steady employment are less likely to live in poverty and more likely to be healthy, many people with steady work still do not earn enough to afford the things they need to stay healthy.Employment programs, career counseling, and high-quality childcare opportunities can help more people find and keep jobs. In addition, policies to help individuals pay for food, housing, health care, and education can reduce poverty and improve health and well-being.
Healthy People 2030 goals:
-
- Economic Stability
- Housing and Homes
- Nutrition and Healthy Eating
- Education Access and Quality
Living in poverty can have an impact on a child’s brain development, leading to classroom challenges. Additionally, children who routinely experience forms of social discrimination like bullying are more likely to struggle with math and reading. Interventions to help children and adolescents do well in school and help families pay for college can have long-term health benefits. Individuals with higher levels of education are more likely to be healthier and live longer.
Healthy People 2030 goals:
-
-
- Adolescents
- Children
- People with Disabilities
- Schools
-
- Health Care Access and Quality
One in 10 people in the United States is uninsured. Individuals without insurance are less likely to have a primary care provider, and they may be unable to afford the health care services and medications they need. Strategies to increase insurance coverage rates are critical for ensuring that more people get essential health care services, like preventive care and treatment for chronic illnesses.
Healthy People 2030 goals:
-
-
- Health Care Access and Quality
- Adolescents
- Cancer
- Community
- Neighborhood and Built Environment
-
The neighborhoods individuals live in significantly affect their health and well-being. Unfortunately, many people in the United States live in neighborhoods with high rates of violence, unsafe air or water, and other health and safety risks. These conditions can be remedied. For example, providing opportunities to walk and bike by adding sidewalks and bike lanes can increase safety and help improve health and quality of life. In addition, many economically vulnerable neighborhoods can be considered food deserts—that is, they areas where people have limited access to a variety of healthy and affordable food. As with other variables that contribute to the health of a community, it is important to understand the characteristics associated with these vulnerable communities, including income, vehicle availability, and access to public transportation. Interventions and policy changes at the local, state, and federal levels can contribute to reducing the risk of these variables to health and safety; at the same time, these policies and strategies can help promote health (United States Department of Agriculture, Economic Research Service, n.d.).
Healthy People 2030 goals:
-
-
-
- Neighborhood and Built Environment—General
- Environmental Health
- Health Policy
- Housing and Homes
- Social and Community Context (Office of Disease Prevention and Health Promotion, 2022)
-
-
Relationships and interactions with family, friends, coworkers, and community members can significantly affect their health and well-being. Many individuals face challenges and dangers they cannot control, like unsafe neighborhoods, discrimination, or trouble affording the things they need.Positive relationships at home, at work, and in the community can help reduce these negative impacts. Interventions to help people get the social and community support they need are critical for improving health and well-being.
Healthy People 2030 goals:
-
-
-
- Social and Community Context—General
- Adolescents
- Health Communication
- LGBT
-
-
The Nurse’s Role in Community Health Advocacy
Nurses are responsible for advocating for policies that advance public health, promote health equity, reduce health disparities, and further social justice. Nurses have an active role to play in understanding the impacts of the policy landscape and in contributing their expertise to the development of policy that affects community health. Targeting SDOH in support of the vulnerable and underserved is advocacy that can significantly promote health. Policy, informed by evidence, can influence improvement in both the social and the economic status of individuals and the community as a whole.
Policy actions in four key social domains have been directly linked with improvements in well-being and reductions in health inequities. These domains comprise child and youth education and development, fair employment and decent work, social protection, and the living environment. Important research has shown that policies can affect health outcomes more than genetic endowment, individual behaviors, or access to health care services can (Carey & Crammond, 2015; Webb, 2014).
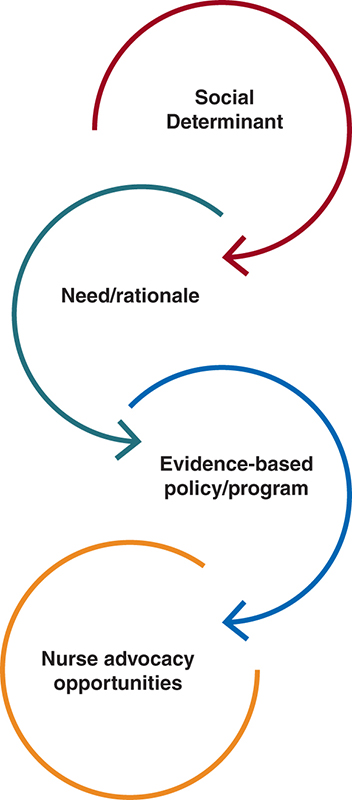
The connection between specific SDOH, examples of evidence-based programs and policies, and related nurse advocacy opportunities are essential to understand. Figure 1.3 illustrates this concept. For instance, in an example adapted from Williams et al. (2018), early childhood is a critical period in a child’s development of personality, cognition, language, and behavior. Early childhood education can be a determinant of health. Children with delayed early childhood development have been linked to issues with depression, attention deficit, and poor academic achievement in school. Evidence-based programs, including early childhood development programs, can serve as intervention strategies to address this. Nurses have the opportunity to advocate for universal access to quality and affordable childcare education services or support publicly funded center-based programs for children 3–5 years of age, for nurses are advocates and experts on these SDOH factors, having seen their impact on the communities they work with (Aron et al., 2015; Webb, 2014).
Practice Application
➔ Setting the Scene
Social Determinants of Health
Watch this video by scanning the QR code or visiting https://youtu.be/u_IoBt7Nicw

➔ Think About It
Imagine you are a community health nurse tasked with supporting the health care of your current community.
- How would you investigate the health policy agendas of your local legislators?
- Drawing on your experience living in the community, what health hazards have you noticed? What would you do to advocate for improvement?
- Develop a set of professional priorities. What social issues would you include?
- Your supervisor has asked you to organize a program to educate the community about SDOH.
- How would you organize this program?
- What would be the key aspects of this program?
- What considerations would you need to incorporate in their community health program design (e.g., health literacy level, language barriers, social or cultural considerations)?
Additional Resources
American Nurses Association Advocacy Resources (Must be a member of ANA to access)
American Association of Colleges of Nursing – Policy and Advocacy
The American Hospital Association – Social Determinants of Health
Healthy People 2030 – Objectives
Health People 2030 – Social Determinants of Health Literature Summaries
National League for Nursing Public Policy Toolkit
Nurse Advocacy: Adopting a Health in All Policies Approach [Article]
References
Agency for Healthcare Quality and Research. (2021). 2021 National healthcare quality and disparities report. https://www.ahrq.gov/research/findings/nhqrdr/nhqdr21/index.html
American Public Health Association. (2021). Social justice and health. https://www.apha.org/what-is-public-health/generation-public-health/our-work/social-justice
Aron, L., Simon, S. M., Dubay, L., Chapman, D., Zimmerman, E., & Woolf, S. H. (2015). Can income-related policies improve population health? (p. 19). https://societyhealth.vcu.edu/media/society-health/pdf/IHIBrief2.pdf
Association of American Medical Colleges (AAMC). (2021). 2021 Fall applicant, matriculant, and enrollment data tables. https://www.aamc.org/media/57761/download
Baciu, A., Negussie, Y., Geller, A., & Weinstein, J. N. (2017). Policies to support community solutions. In National Academies of Sciences, Engineering, and Medicine; Health and Medicine (Ed.), Policies to support community solutions (pp. 335–382). National Academies Press (US). https://www.ncbi.nlm.nih.gov/books/NBK425843/
Benjamin, R. (2018). Health policy affects health outcomes: Community determinants of health. Progress in community health partnerships. Research, Education, and Action, 12(1 Suppl.), 1–2. https://doi.org/10.1353/cpr.2018.0012
Braveman, P. A., Kumanyika, S., Fielding, J., LaVeist, T., Borrell, L. N., Manderscheid, R., & Troutman, A. (2011). Health disparities and health equity: The issue is justice. American Journal of Public Health, 101(Suppl. 1), S149–S155. https://doi.org/10.2105/AJPH.2010.300062
Campaign for Action. (2022). New RN graduates by degree type, by race/ethnicity. Retrieved March 29, 2024, from https://campaignforaction.org/resource/new-rn-graduates-degree-type-raceethnicity/
Carey, G., & Crammond, B. (2015). Action on the social determinants of health: Views from inside the policy process. Social Science & Medicine, 128, 134–141. https://doi.org/10.1016/j.socscimed.2015.01.024
Centers for Disease Control and Prevention. (2021, March 10). About social determinants of health (SDOH). https://www.cdc.gov/about/priorities/why-is-addressing-sdoh-important.html
Civil Rights Act of 1964, Pub. L. No. 88-352, 78 Stat. 241 (1964). https://www.govinfo.gov/content/pkg/STATUTE-78/pdf/STATUTE-78-Pg241.pdf
Cohen, J. J., Gabriel, B. A., & Terrell, C. (2002). The case for diversity in the health care workforce. Health Affairs, 21(5), 90–102. https://doi.org/10.1377/hlthaff.21.5.90
Gostin, L. (1995). The formulation of health policy by the three branches of government. In Institute of Medicine, R. E. Bulger, E. M. Bobby, & H. V. Fineberg (Eds.), The formulation of health policy by the three branches of government. National Academies Press (US). https://www.ncbi.nlm.nih.gov/books/NBK231979
Heckler, M. (1986). Report of the secretary’s task force on Black & minority health. U.S. Dept. of Health and Human Services. https://collections.nlm.nih.gov/catalog/nlm:nlmuid-8602912-mvset
Keller, T., & Ridenour, N. (2021). Ethics. In J. Giddens (Ed.), Concepts for nursing practice. Elsevier.
Office of Disease Prevention and Health Promotion. (n.d.). Healthy People 2030: Social determinants of health. Retrieved January 9, 2024, from https://health.gov/healthypeople/priority-areas/social-determinants-health
Office of Disease Prevention and Health Promotion. (2022). Healthy People 2030. https://health.gov/healthypeople
Rieck, G., & Lundin, J. (2018). Health education. https://oercommons.org/courses/health-science
United States Department of Agriculture, Economic Research Service. (n.d.). Food access research atlas. Retrieved April 9, 2024, from https://www.ers.usda.gov/data-products/food-access-research-atlas/
U.S. Department of Health and Human Services. (2021). Serving vulnerable and underserved populations. https://www.hhs.gov/guidance/sites/default/files/hhs-guidance-documents/006_Serving_Vulnerable_and_Underserved_Populations_0.pdf
Webb, B. C. (2014, April 3). Moving upstream: Policy strategies to address social, economic, and environmental conditions that shape health inequities. Joint Center for Political and Economic Studies. https://jointcenter.org/moving-upstream-policy-strategies-to-address-social-economic-and-environmental-conditions-that-shape-health-inequities/
Williams, S. D., Phillips, J. M., & Koyama, K., (2018, September 30). Nurse advocacy: Adopting a health in all policies approach. OJIN: The Online Journal of Issues in Nursing, 23(3), Manuscript 1. https://doi.org/10.3912/OJIN.Vol23No03Man01

