Chapter Two: Health Disparities and Health Equity
Overview
This chapter introduces the concepts of health inequities, health disparity, and health equity. Inequities are differences in treatment that are unfair or unjust. When applied to health care, the term inequity can mean unfair treatment from health providers or unequal access to care or quality health care. Disparities are the differences in outcomes between groups of people. When the term is applied to health, disparity means that there are differences in the state of health between populations that are rooted in unequal treatment or social conditions.
Learning Objectives
- Understand the difference between health disparities and health equity
- Discuss health care inequity
- Recognize how history shapes current health care quality and health outcomes
- Identify the impact that health disparities have on individuals and communities
- Discuss the nurse’s role in promoting health equity
- Compare and contrast health outcomes between historically excluded aggregates and those with historical social advantage
Key Terms
- health equity
- health disparity
- immigrant
- asylum seeker
- refugee
- ableism
- LGBTQIA+
Introduction
Health disparities and health equity have a profound influence on health and quality of health care received by individuals. Health equity is a fair and just treatment that promotes the prevention or correction of health disparities. Health equity can be achieved through individual actions in providing unbiased, culturally sensitive care and through ensuring equitable access to health care. There are historical, social, economic, and structural (or systemwide) barriers to providing equitable care. These systemic barriers can be remedied through actions that promote health justice.
Health Equity, Inequities, and Disparities
Health equity is achieved when every person has the opportunity to “attain [their] full health potential, [and no one is] disadvantaged from achieving this potential because of social position or other socially determined circumstances” (Centers for Disease Control and Prevention [CDC], 2022b). Health care inequities are the differences in the distribution of health care resources between population groups, arising from the sociopolitical, economic, and structural conditions in which people are born, grow, live, work, and age. The term health care inequality is often used interchangeably with health care inequities; however, as indicated in Figure 2.1, the two terms are vastly different. Equality means everyone is given the same resources, whereas equity recognizes that each person has different circumstances and needs different resources to reach the same outcome.
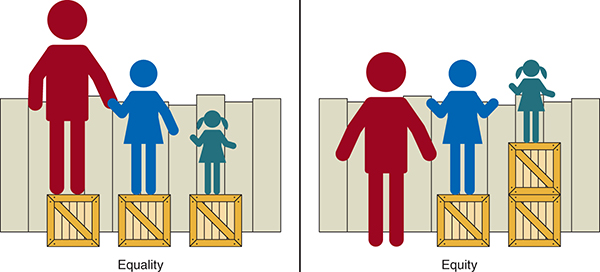
Long Description for Figure 2.1
On the left side, equality is represented. Three figures of different heights standing on identical wooden boxes beside a fence. While the taller figures can see over the fence, the shortest figure cannot see over the fence. On the right side, equity is represented using the same three figures standing on boxes, but the boxes are distributed differently. The tallest figure stands on the ground without a box. The shortest figures stand on two boxes stacked one over the other. The figure of intermediary height stands on one box. Now, all three figures can see over the fence.
Health care inequities are the systemic issues that contribute to poor health outcomes and lead to health disparities (World Health Organization, 2022). Health disparities are the differences that exist among specific population groups in the attainment of good health. These differences can be measured by examining health outcomes, including incidence, prevalence, mortality, the burden of disease, and other adverse health conditions (National Academies of Sciences et al., 2017). Working toward health equity means that we must work to reduce health care inequities and health disparities. We need to address why health differences persist, and in so doing, we must evaluate the social-ecological factors that have contributed to the disparities. As health care professionals, we need to expand our perspectives and recognize that issues within our health system and in the health of our patients are reflections of society. This means that we must proactively address discrimination to improve population health.
People are treated differently for many reasons, including racism, sexism, socioeconomic discrimination, and ableism. “Ableism is the discrimination of and social prejudice against people with disabilities based on the belief that typical abilities are superior. At its heart, ableism is rooted in the assumption that disabled people require ‘fixing’ and defines people by their disability. Like racism and sexism, ableism classifies entire groups of people as ‘less than’ and includes harmful stereotypes, misconceptions, and generalizations of people with disabilities” (Eisenmenger, 2019).
In addition to being treated differently, these same populations are more likely to experience a lack of patient–provider concordance, contributing to lower quality of care and differences in health attainment. Health care organizations have a growing responsibility to improve diversity, equity, and inclusion (DEI) in employment to serve patients and their families better. One strategy is to diversify the nursing workforce, which comprises the largest number of health care professions. With nursing strategically positioned to provide care to diverse groups, in addition to diversifying the nursing workforce, measures must also be taken to address bias, stereotyping, and clinical uncertainty (Shen et al., 2018).
Health disparities tend to be persistent and difficult to change for many reasons. The dynamic interrelationships between the physical environment, political landscape, social and cultural environment, and personal attributes play a key role in health, health care, and well-being. Health disparities and substandard public health carry societal, economic, and individual health implications for all citizens, and it is necessary to focus on solutions to decrease health care inequities and health disparities.
Research Framework for Health Disparities
To address health care disparities and inequities and improve patient outcomes for all populations, a research framework was developed by the National Institutes of Health’s National Institute on Minority Health and Health Disparities (NIMHD; Table 2.1). This framework is used to help us understand and promote the health of minorities to reduce health disparities. It does this by encouraging researchers to include diverse communities in their research and understand the domains of influence and their impact on health outcomes (Agency for Healthcare Research and Quality, 2021).
|
Levels of Influence |
|||||
|---|---|---|---|---|---|
|
Domains influence (over the life course) |
Individual |
Interpersonal |
Community |
Societal |
|
|
Biological |
Biological vulnerability and mechanisms |
Caregiver–child interaction Family microbiome |
Community illness Exposure Herd immunity |
Sanitation Immunization Pathogen exposure |
|
|
Behavioral |
Health behaviors Coping strategies |
Family functioning School/work functioning |
Community functioning |
Policies and laws |
|
|
Physical/Built Environment |
Personal environment |
Household environment School/work environment |
Community environment Community resources |
Societal structure |
|
|
Sociocultural Environment |
Sociodemographics Limited English Cultural identity Response to discrimination |
Social networks Family/peer norms Interpersonal discrimination |
Community norms Local structural discrimination |
Social norms Societal structures Discrimination |
|
|
Health care system |
Insurance coverage Health literacy Treatment preferences |
Patient-clinician relationship Medical decision-making |
Availability of services Safety net services |
Quality of care Health care policies |
|
|
Health outcomes |
 |
 |
 |
 |
|
Impact of Health Disparities
Racial and Ethnic Minorities
In the United States, the impact of structural racism has continued far beyond the formal end of slavery in 1865. Following the Civil War, discriminatory laws favored majority populations and prevented minority populations from having a full and equal opportunity to participate in the political process that determined the reach of those laws and policies. Segregation ensured that Black and immigrant populations were restricted to living in socioeconomically disadvantaged neighborhoods. Redlining, a process that marked such neighborhoods as too risky for financial investments (including mortgages and small-business loans), limited residents’ access to resources to improve their socioeconomic status. With these structural disadvantages came decreased access to health care and overall lower quality of care, because clinics, hospitals, and medical centers were located elsewhere, and the cost of quality care was out of reach for many.
As recently as 2002, the Institute of Medicine reported that even when controlled for lack of health insurance and access to health care, racial and ethnic minorities tend to receive a lower quality of care. Racism and discrimination have been shown to have a negative influence on disease burden within communities, including higher rates of heart disease, cancer, diabetes, obesity, depression, infant mortality, and maternal morbidity (Hawkins et al., 2022). Table 2.2 shows the number of measures for which specific racial or ethnic groups have better, same, or worse care compared with White groups. Compared with White groups, the number of worse measures exceeded the number of measures better for all racial and ethnic minority groups except Asian groups. Some health care disparities, such as those related to HIV outcomes, were common to most racial and ethnic minority groups. Other health care disparities were more prominent for certain groups, reflecting specific contexts and issues experienced by that group. Each racial or ethnic minority group has experienced improving care for many measures, but significant disparities persist because White populations experienced similarly improving care. Since 2000, disparities have narrowed to only about 8% of measures for American Indian and Alaska Native populations, 2% of measures for Asian populations, 3% of measures for Black populations, 4% of measures for Hispanic populations, and 10% of measures of Native Hawaiian/Pacific Islander populations (Agency for Healthcare Research and Quality, 2021).
|
Race or Ethnic Group |
Better |
Same |
Worse |
|---|---|---|---|
|
American |
12 (11%) |
53 (49%) |
43 (40%) |
|
Asian |
50 (29%) |
75 (43%) |
48 (28%) |
|
Black |
21 (11%) |
90 (46%) |
84 (43%) |
|
Hispanic |
34 (20%) |
76 (44%) |
62 (36%) |
|
Native/Hawaiian/Pacific Islander |
15 (19%) |
43 (53%) |
23 (28%) |
Women
Women are another group that experiences avoidable disparities. Globally, women have differing levels of freedom, autonomy, and self-determination. The right to vote in the United States was expanded to White women in 1926 and Black women in 1965 (National Archives, 2015). Yet, American women did not have the right to open bank accounts until the Equal Opportunity Credit Act of 1974 (GovTrack, 2022). Societal measures such as these kept women dependent on male family members. Economic disparities and limited access to equitable health care persist for women, in particular for women in historically underserved populations.
Women experience many unique health issues—for example, pregnancy, childbirth, and menopause. Moreover, some health issues that affect both men and women pose unique challenges for women. Healthy People 2030 focuses on addressing these specific needs to improve women’s health and safety throughout their lives (U.S. Office of Disease Prevention and Health Promotion [ODPHP], 2022).
Women are also at risk for diseases such as breast and cervical cancer. Screening for these diseases and health issues that disproportionately affect women is key to identifying problems and making sure women get the treatment they need (ODPHP, 2022).
Both pregnancy and childbirth can lead to serious long-term health problems for women. Strategies to decrease unplanned pregnancies and make sure women get high-quality health care before, during, and after pregnancy can help reduce serious health problems and deaths (ODPHP, 2022). Reproductive justice is essential to reducing inequities and ensuring consistent, high-quality care for all women. More information about reproductive health care can be found in Chapter 11.
LGBTQIA+
Another marginalized group comprises members of the lesbian, gay, bisexual, transgender, questioning/queer, intersex, and asexual (LGBTQIA+) community. According to healthypeople.gov, research suggests that LGBTQIA+ individuals face health disparities linked to societal stigma, discrimination, and denial of their civil and human rights. Discrimination against LGBTQIA+ persons has been associated with high rates of psychiatric disorders, substance abuse, and suicide. Experiences of violence and victimization are frequent for LGBTQIA+ individuals and have long-lasting effects on the individual and the community. Personal, family, and social acceptance of sexual orientation and gender identity affects the mental health and personal safety of LGBTQIA+ individuals (ODPHP, n.d.). According to youth.gov, LGBTQIA+ youth are far more likely to experience housing insecurity, which can have a resoundingly negative effect on health and well-being (Youth.gov, n.d.). The perspectives and needs of LGBTQIA+ people should be routinely considered in public health efforts to improve the overall health of every person and eliminate health disparities (CDC, 2022c).
Disability
As of 2016, in the United States an estimated one in four adults, or 61 million people, reported a disability. Individuals with disabilities (such as mobility limitations, deafness, blindness, or intellectual disabilities) face many challenges in achieving optimal health and accessing high-quality health care.
Asylees, Immigrants, Migrants, and Refugees
There is a difference between immigrant, asylee, and refugee status. Although each of these terms applies to people who have left their home country to enter another country, there are similar yet unique health challenges associated with each. An immigrant is any person who is lawfully in the United States who is not a U.S. citizen, U.S. national, or person admitted under a nonimmigrant category as defined by the Immigration and Nationality Act, Section 101 (a) (15), passed by the U.S. House of Representatives (U.S. Code, 2024). With the word lawfully placed in the definition provided by Homeland Security, those individuals not lawfully present in the United States are referenced in the literature as “undocumented.” This is important to recognize in terms of access to care- and health-seeking behaviors. Undocumented immigrants are often barred access to insurance by law. And though documented immigrants can acquire health insurance, they may nonetheless face barriers in obtaining health care, such as difficulties communicating with a provider or experiencing cultural challenges (Hacker et al., 2015). Migrants are persons who leave their country of origin to seek temporary or permanent residence in another country, specifically with migrant status. An asylee, or asylum seeker, is an immigrant who has been forcibly displaced and might have fled their home country because of war or other factors harming them or their family. Seeking asylum or sanctuary is a legal process. Once a government has accepted an asylum seeker, the seeker’s status becomes that of a refugee and hence becomes lawful. Deferred Action for Childhood Arrivals, or DACA, recipients are another group at risk of facing inequities. President Obama created this program in 2012 to protect from deportation people who were brought to the United States as children and who did not have citizenship or legal residency. The protection has to be renewed every 2 years and is not yet a pathway to citizenship. Recipients of DACA can get work permits and obtain health insurance from employers. However, in most states DACA recipients cannot get health insurance through the health care exchange (Jordan, 2022).
Health disparities among immigrants exist for many reasons. A study by the Robert Wood Johnson Foundation (2017) indicated that immigrants have lower rates of health insurance, have lower rates of health care use, and experience lower quality of care than do U.S. citizens and those born in the country. Some immigrants, with or without green card status, experience high levels of long-term stress associated with deportation fears, affecting their physical and mental health (Robert Wood Johnson Foundation, 2017). The effects of toxic stress are more pronounced in children, where it may cause barriers to normal physical and mental growth and development. Fear of deportation also influences associated health-seeking behaviors such as seeking out assistance to prevent food insecurity or housing insecurity (Robert Wood Johnson Foundation, 2017).
Health care professionals can intervene by providing unbiased care, referral to the United Nations High Commissioner for Refugees to establish legal status, and case management services to access services and entitlements, such as SNAP, the Supplemental Nutrition Assistance Program. Nurses should be careful to provide written materials in the patient’s native language and to use medical translation services. Nurses should also advocate for funding programs that serve such underserved populations as immigrants. Ensuring workforce diversity and leadership development opportunities for nurses who are from racially and ethnically underrepresented groups must remain a high priority to eliminate health disparities and, ultimately, achieve health equity (Institute of Medicine, 2001).
The Nurse’s Role in Promoting Health Equity
The American Nurses Association’s Code of Ethics (2021) obligates nurses to speak up against racism, discrimination, and injustice and to advocate for their patients. Nurses must work to integrate equity into their delivery of care from the individual level to the systems level. Furthermore, nurses must examine their own biases. Addressing social needs in the clinical setting and within the community, working with other disciplines to simultaneously meet a variety of patient needs, and advocating for policy change are all a part of the nurse’s role in promoting health equity (National Academies of Sciences et al., 2021; American Association of Colleges of Nursing, 2024).
The Future of Nursing Report (National Academies of Sciences et al., 2021) calls for nurses to reduce health disparities and prioritize achieving health equity. Achieving health equity requires valuing everyone equally with focused and ongoing societal efforts to address avoidable inequalities and historical and contemporary injustices and eliminate health and health care disparities. Achieving health equity also involves acknowledging and addressing racism as a threat to public health and the history of unethical practices in public health that lead to inequitable health outcomes (CDC, 2023).
The AACN Essentials (American Association of Colleges of Nursing, 2021) specifically call for nurses to “design policies to impact health equity and structural racism within systems, communities, and populations” and advocate for the promotion of social justice and eradication of structural racism and systematic inequity in nursing and society.”
Nurses play an essential role in addressing health equity by engaging in these important activities:
- Creating inclusive environments that acknowledge and challenge racism in all aspects of nursing education and professional practice
- Advocating for social policies that promote health care equity at the community, state, and national level
- Participating experiential learning opportunities in communities where care is needed
- Prioritizing reducing health disparities among populations disproportionately affected by HIV, viral hepatitis, sexually transmitted infections, tuberculosis, and other related conditions
- Intentionally recruiting, supporting, and mentoring nursing students and nurses from diverse backgrounds to ensure that the next generation of nurses reflects the communities they serve (National Academies of Sciences et al., 2021)
Nurses must be committed to the equitable delivery of care from the individual level to the systems level.
Practice Application
➔ Setting the Scene
A 37-year-old male comes to a community clinic complaining of unintentional weight loss of 20 pounds over the last 2 months, abdominal bloating, severe fatigue, and persistent gastroesophageal reflux disease (GERD). The provider determines that the patient needs a colonoscopy. The patient is uninsured and, on further discussion with the provider, shared that he is a DACA recipient and is currently unemployed. He states that he tried to get health insurance through the health care exchange but was denied because of his DACA status.
➔ Think About It
Imagine you are the nurse assisting this patient.
- How would you (or would you not) proceed with offering care to this patient? Why?
- What other health disparities might this patient experience because of his DACA status?
- What additional health disparities might this patient experience if he were part of other marginalized groups, such as racial minorities or LBGTQIA+?
- What effect does being a part of multiple-impacted communities have on the health disparities an individual might experience?
- How might addressing health disparities among underserved populations of people, like this patient, help promote health equity on a larger scale?
Additional Resources
Health Equity
American Planning Association – Plan for Health
American Planning Association – Planners for Health
CDC, Division of Nutrition, Physical Activity, and Obesity – Health Equity Resource
MPHI – Equity in Action Workshops
University of Wisconsin-Madison, Population Health Institute – Health Equity Training Modules
References
Agency for Healthcare Research and Quality. (2021). 2021 National healthcare quality and disparities report. www.ahrq.gov/research/findings/nhqrdr/nhqdr21/index.html
American Association of Colleges of Nursing. (2021). The essentials: Core competencies for professional nursing education.
American Nurses Association. (2021). ANA code of ethics. https://www.nursingworld.org/practice-policy/nursing-excellence/ethics/code-of-ethics-for-nurses/
American Association of Colleges of Nursing. (2024). Health equity. 5B tool kit. https://www.aacnnursing.org/5b-tool-kit/themes/health-equity#:~:text=The%20AACN%20Essentials%20(2021)%20specifically,inequity%20in%20nursing%20and%20society
Centers for Disease Control and Prevention. (2022b, March 3). Health equity. www.cdc.gov/chronicdisease/healthequity/index.htm
Centers for Disease Control and Prevention. (2022c, July 27). Lesbian, gay, bisexual, and transgender health. https://web.archive.org/web/20240207175332/http://www.cdc.gov/lgbthealth/index.htm
Centers for Disease Control and Prevention. (2023, January 9). What is health equity? https://www.cdc.gov/nchhstp/healthequity/index.html
Eisenmenger, A. (2019, December 12). Ableism 101—What is ableism? What does it look like? Access Living. accessliving.org/newsroom/blog/ableism-101/
GovTrack. (2022). S. 3492—93rd Congress: Equal Credit Opportunity Act of 1974. https://www.govtrack.us/congress/bills/93/s3492
Hacker, K., Anies, M., Folb, B. L., & Zallman, L. (2015). Barriers to health care for undocumented immigrants: a literature review. Risk management and healthcare policy, 8, 175–183. https://doi.org/10.2147/RMHP.S70173
Hawkins, J., Hoglund, L., Martin, J. M., Chiles, M. T., & Tufts, K. A. (2022). Antiracism and health: an action plan for mitigating racism in healthcare. In Developing anti-racist practices in the helping professions: inclusive theory, pedagogy, and application (pp. 421–450). Springer.
Institute of Medicine (US) Committee on the Consequences of Uninsurance. (2001). Coverage matters: Insurance and health care. National Academies Press (US). www.ncbi.nlm.nih.gov/books/NBK223654/
Jordan, M. (2022, June 14). What is DACA? And where does it stand now? The New York Times. www.nytimes.com/article/what-is-daca.html
National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Population Health and Public Health Practice; Committee on Community-Based Solutions to Promote Health Equity in the United States; Baciu, A., Negussie, Y., Geller, A., & Weinstein, J. N. (Eds.). (2017). The state of health disparities in the United States. In Communities in action: Pathways to health equity. National Academies Press (US). www.ncbi.nlm.nih.gov/books/NBK425844/
National Academies of Sciences, Engineering, and Medicine; National Academy of Medicine; Committee on the Future of Nursing 2020–2030. Flaubert, J. L., Le Menestrel, S., Williams, D. R., & Wakefield, M. K. (Eds.). (2021). The future of nursing 2020–2030: Charting a path to achieve health equity. National Academies Press (US). https://doi.org/10.17226/25982
National Institutes of Health. (2022). Implicit bias. https://diversity.nih.gov/sociocultural-factors/implicit-bias
Office of Disease Prevention and Health Promotion. (n.d.). Lesbian, gay, bisexual, and transgender health. Healthy People 2020. Retrieved August 23, 2022, from https://www.wpath.org/soc8
Office of Disease Prevention and Health Promotion. (2022). Healthy People 2030: Women. health.gov/healthypeople/objectives-and-data/browse-objectives/women
Robert Wood Johnson Foundation. (2017, September 12). Immigration, health care and health. www.rwjf.org/en/library/research/2017/09/immigration-status-and-health.html
Shen, M. J., Peterson, E. B., Costas-Muñiz, R., Hernandez, M. H., Jewell, S. T., Matsoukas, K., & Bylund, C. L. (2018). The effects of race and racial concordance on patient–physician communication: A systematic review of the literature. Journal of Racial and Ethnic Health Disparities, 5(1), 117–140. https://doi.org/10.1007/s40615-017-0350-4
US Code (2024). 8 usc 1101: Definitions. (n.d.). Retrieved April 15, 2024, from https://uscode.house.gov/view.xhtml?req=granuleid:USC-prelim-title8-section1101&num=0&edition=prelim
World Health Organization. (2022). Health inequities and their causes. www.who.int/news-room/facts-in-pictures/detail/health-inequities-and-their-causes
Youth.gov. (n.d.). Homelessness and housing. Retrieved August 23, 2022, from youth.gov/youth-topics/lgbtq-youth/homelessness

