18 Chapter 18 The Cardiovascular System: Blood
By Rajeev Chandra
Motivation.
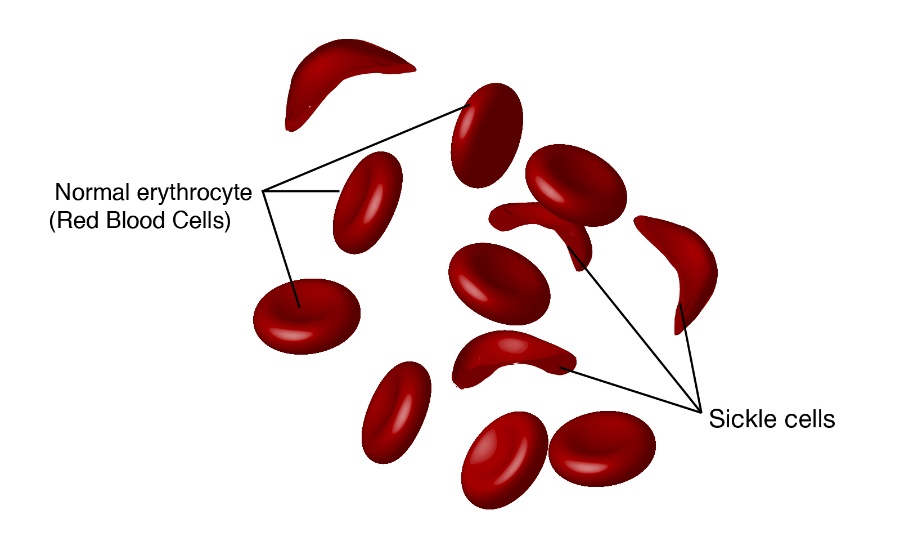
Sickle cell disease is a group of inherited red blood cell disorders most common in the United States. Approximately 100,000 Americans have the disease. In the United States, sickle cell disease is most prevalent among African Americans. About one in 12 African Americans carry the sickle cell trait, which means they are carriers of the disease.
Sickle cell disease is caused by a mutation in the hemoglobin-beta gene found on chromosome 11. Hemoglobin transports oxygen from the lungs to other parts of the body. Red blood cells with normal hemoglobin (hemoglobin-A) are smooth and round and glide through blood vessels. In people with sickle cell disease, abnormal hemoglobin molecules – hemoglobin S – stick to one another and form long, rod-like structures. These structures cause red blood cells to become stiff, assuming a sickle shape. Their shape causes these red blood cells to pile up, causing blockages and damaging vital organs and tissue.
Sickle cells are destroyed rapidly in the bodies of people with the disease, causing anemia. This anemia is what gives the disease its commonly known name – sickle cell anemia. The sickle cells also block the flow of blood through vessels, resulting in lung tissue damage that causes acute chest syndrome, pain episodes, stroke and priapism (painful, prolonged erection). It also causes damage to the spleen, kidneys and liver. The damage to the spleen makes patients – especially young children – easily overwhelmed by bacterial infections.
Learning Objectives
Upon completion of the work in this chapter students should be able to:
- Name the major components of blood and identify the percentage of each present in whole blood.
- Compare and contrast red blood cells, leukocytes, and platelets microscopically
- Classify the white blood cells (leukocytes) based on microscopic structure and function
- Conduct ABO and Rh blood typing on simulated blood samples, and state the importance of this test
Background.
Recall that blood is a connective tissue. Like all connective tissues, it is made up of cellular elements and an extracellular matrix. The cellular elements—referred to as the formed elements—include red blood cells (RBCs), white blood cells (WBCs), and cell fragments called platelets. The extracellular matrix, called plasma, makes blood unique among connective tissues because it is fluid. This fluid, which is mostly water, perpetually suspends the formed elements and enables them to circulate throughout the body within the cardiovascular system.
Functions of Blood
The primary function of blood is to deliver oxygen and nutrients to and remove wastes from body cells, but that is only the beginning of the story. The specific functions of blood also include defense, distribution of heat, and maintenance of homeostasis.
Transportation
Nutrients from the foods you eat are absorbed in the digestive tract. Most of these travel in the bloodstream directly to the liver, where they are processed and released back into the bloodstream for delivery to body cells. Oxygen from the air you breathe diffuses into the blood, which moves from the lungs to the heart, which then pumps it out to the rest of the body. Moreover, endocrine glands scattered throughout the body release their products, called hormones, into the bloodstream, which carries them to distant target cells. Blood also picks up cellular wastes and byproducts, and transports them to various organs for removal. For instance, blood moves carbon dioxide to the lungs for exhalation from the body, and various waste products are transported to the kidneys and liver for excretion from the body in the form of urine or bile.
Defense
Many types of WBCs protect the body from external threats, such as disease-causing bacteria that have entered the bloodstream in a wound. Other WBCs seek out and destroy internal threats, such as cells with mutated DNA that could multiply to become cancerous, or body cells infected with viruses.
When damage to the vessels results in bleeding, blood platelets and certain proteins dissolved in the plasma, the fluid portion of the blood, interact to block the ruptured areas of the blood vessels involved. This protects the body from further blood loss.
Maintenance of Homeostasis
Recall that body temperature is regulated via a classic negative-feedback loop. If you were exercising on a warm day, your rising core body temperature would trigger several homeostatic mechanisms, including increased transport of blood from your core to your body periphery, which is typically cooler. As blood passes through the vessels of the skin, heat would be dissipated to the environment, and the blood returning to your body core would be cooler. In contrast, on a cold day, blood is diverted away from the skin to maintain a warmer body core. In extreme cases, this may result in frostbite.
Blood also helps to maintain the chemical balance of the body. Proteins and other compounds in blood act as buffers, which thereby help to regulate the pH of body tissues. Blood also helps to regulate the water content of body cells.
Composition of Blood
You have probably had blood drawn from a superficial vein in your arm, which was then sent to a lab for analysis. Some of the most common blood tests—for instance, those measuring lipid or glucose levels in plasma—determine which substances are present within blood and in what quantities. Other blood tests check for the composition of the blood itself, including the quantities and types of formed elements.
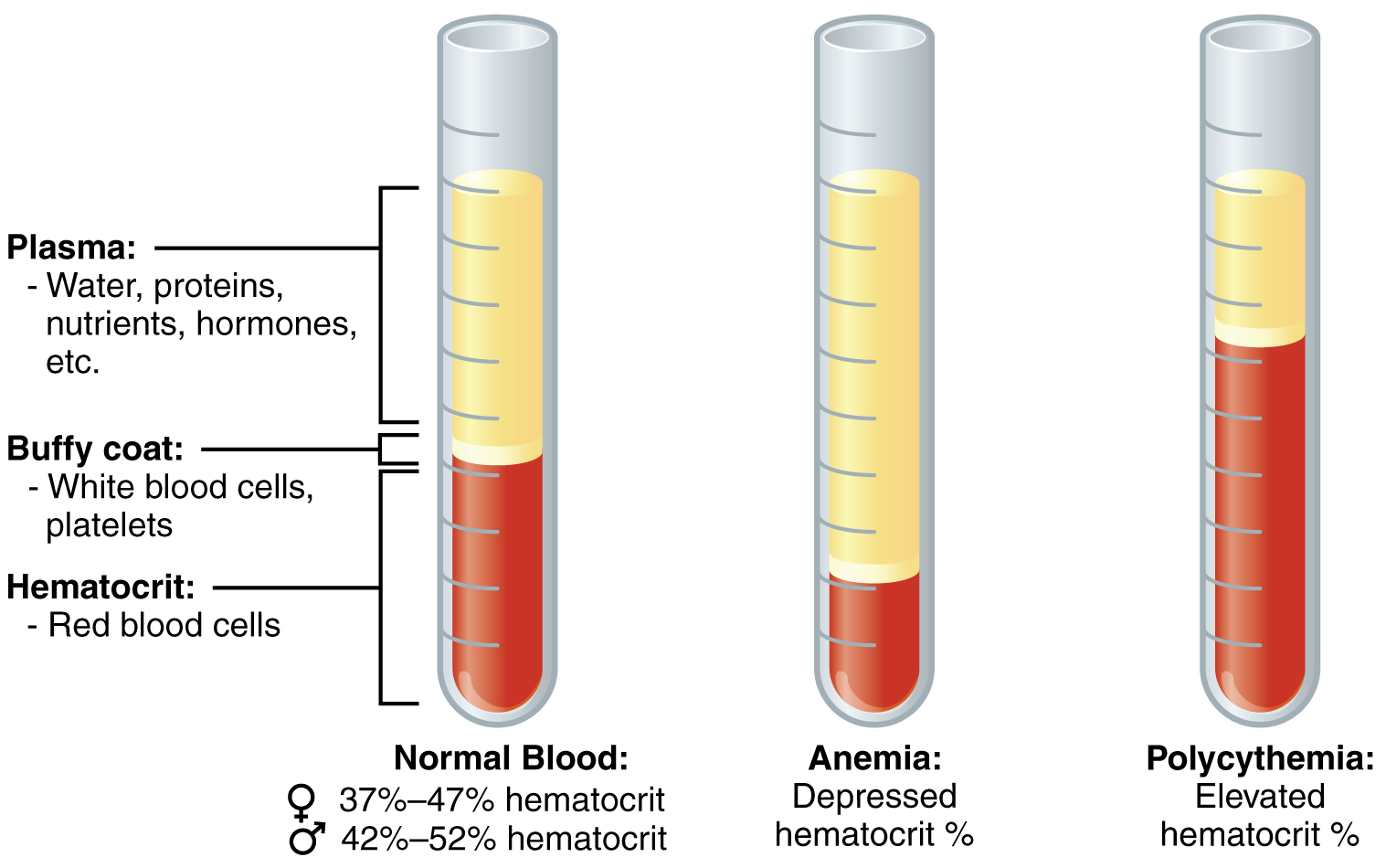
One such test, called a hematocrit, measures the percentage of RBCs, clinically known as erythrocytes, in a blood sample. It is performed by spinning the blood sample in a specialized centrifuge, a process that causes the heavier elements suspended within the blood sample to separate from the lightweight, liquid plasma (Figure 18.2). Because the heaviest elements in blood are the erythrocytes, these settle at the very bottom of the hematocrit tube. Located above the erythrocytes is a pale, thin layer composed of the remaining formed elements of blood. These are the WBCs, clinically known as leukocytes, and the platelets, cell fragments also called thrombocytes. This layer is referred to as the buffy coat because of its color; it normally constitutes less than 1 percent of a blood sample. Above the buffy coat is the blood plasma, normally a pale, straw-colored fluid, which constitutes the remainder of the sample.
The volume of erythrocytes after centrifugation is also commonly referred to as packed cell volume (PCV). In normal blood, about 45 percent of a sample is erythrocytes. The hematocrit of any one sample can vary significantly, however, about 36–50 percent, according to gender and other factors. Normal hematocrit values for females range from 37 to 47, with a mean value of 41; for males, hematocrit ranges from 42 to 52, with a mean of 47. The percentage of other formed elements, the WBCs and platelets, is extremely small so it is not normally considered with the hematocrit. So the mean plasma percentage is the percent of blood that is not erythrocytes: for females, it is approximately 59 (or 100 minus 41), and for males, it is approximately 53 (or 100 minus 47).
Composition of Blood
Characteristics of Blood
When you think about blood, the first characteristic that probably comes to mind is its color. Blood that has just taken up oxygen in the lungs is bright red, and blood that has released oxygen in the tissues is a more dusky red. This is because hemoglobin is a pigment that changes color, depending upon the degree of oxygen saturation.
Blood is viscous and somewhat sticky to the touch. It has a viscosity approximately five times greater than water. Viscosity is a measure of a fluid’s thickness or resistance to flow, and is influenced by the presence of the plasma proteins and formed elements within the blood. The viscosity of blood has a dramatic impact on blood pressure and flow. Consider the difference in flow between water and honey. The more viscous honey would demonstrate a greater resistance to flow than the less viscous water. The same principle applies to blood.
The normal temperature of blood is slightly higher than normal body temperature—about 38 °C (or 100.4 °F), compared to 37 °C (or 98.6 °F) for an internal body temperature reading, although daily variations of 0.5 °C are normal. Although the surface of blood vessels is relatively smooth, as blood flows through them, it experiences some friction and resistance, especially as vessels age and lose their elasticity, thereby producing heat. This accounts for its slightly higher temperature.
The pH of blood averages about 7.4; however, it can range from 7.35 to 7.45 in a healthy person. Blood is therefore somewhat more basic (alkaline) on a chemical scale than pure water, which has a pH of 7.0. Blood contains numerous buffers that actually help to regulate pH.
Blood constitutes approximately 8 percent of adult body weight. Adult males typically average about 5 to 6 liters of blood. Females average 4–5 liters.
Blood Plasma
Like other fluids in the body, plasma is composed primarily of water: In fact, it is about 92 percent water. Dissolved or suspended within this water is a mixture of substances, most of which are proteins. There are literally hundreds of substances dissolved or suspended in the plasma, although many of them are found only in very small quantities.
Visit this site for a list of normal levels established for many of the substances found in a sample of blood. Serum, one of the specimen types included, refers to a sample of plasma after clotting factors have been removed. What types of measurements are given for levels of glucose in the blood?
Plasma Proteins
About 7 percent of the volume of plasma—nearly all that is not water—is made of proteins. These include several plasma proteins (proteins that are unique to the plasma), plus a much smaller number of regulatory proteins, including enzymes and some hormones.
The three major groups of plasma proteins are as follows:
- Albumin is the most abundant of the plasma proteins. Manufactured by the liver, albumin molecules serve as binding proteins—transport vehicles for fatty acids and steroid hormones. Recall that lipids are hydrophobic; however, their binding to albumin enables their transport in the watery plasma. Albumin is also the most significant contributor to the osmotic pressure of blood; that is, its presence holds water inside the blood vessels and draws water from the tissues, across blood vessel walls, and into the bloodstream. This in turn helps to maintain both blood volume and blood pressure. Albumin normally accounts for approximately 54 percent of the total plasma protein content, in clinical levels of 3.5–5.0 g/dL blood.
- The second most common plasma proteins are the globulins. A heterogeneous group, there are three main subgroups known as alpha, beta, and gamma globulins. The alpha and beta globulins transport iron, lipids, and the fat-soluble vitamins A, D, E, and K to the cells; like albumin, they also contribute to osmotic pressure. The gamma globulins are proteins involved in immunity and are better known as an antibodies or immunoglobulins. Although other plasma proteins are produced by the liver, immunoglobulins are produced by specialized leukocytes known as plasma cells. (Seek additional content for more information about immunoglobulins.) Globulins make up approximately 38 percent of the total plasma protein volume, in clinical levels of 1.0–1.5 g/dL blood.
- The least abundant plasma protein is fibrinogen. Like albumin and the alpha and beta globulins, fibrinogen is produced by the liver. It is essential for blood clotting, a process described later in this chapter. Fibrinogen accounts for about 7 percent of the total plasma protein volume, in clinical levels of 0.2–0.45 g/dL blood.
Other Plasma Solutes. In addition to proteins, plasma contains a wide variety of other substances. These include various electrolytes, such as sodium, potassium, and calcium ions; dissolved gases, such as oxygen, carbon dioxide, and nitrogen; various organic nutrients, such as vitamins, lipids, glucose, and amino acids; and metabolic wastes. All of these nonprotein solutes combined contribute approximately 1 percent to the total volume of plasma.
The components of whole blood are plasma (the liquid matrix), accounting for 55% of the volume, and the formed elements (red blood cells, white blood cells and platelets), which account for the remaining 45% of volume. Plasma is a straw-colored liquid consisting of 90% water, salts and proteins that are important for maintaining osmotic balance, buffering against pH changes, maintaining blood viscosity, transporting certain materials, and for blood clotting when a blood vessel is injured. There are three major formed elements – red blood cells (erythrocytes), white blood cells (leukocytes), and platelets (which are cell fragments).
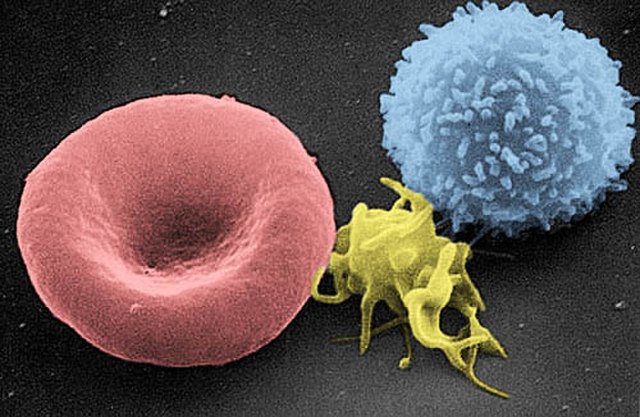
Red blood cells, the most numerous cells in the blood, carry oxygen from the lungs to all parts of the body. A red blood cells is a biconcave disk with a thin center, a shape that provides a large surface area for efficient diffusion of oxygen, and the flexibility to pass through even the smallest blood vessels. Red blood cells contain the protein hemoglobin which has an iron ion incorporated into its structure. When blood travels through the lungs, the oxygen in the lungs combines with the iron in the hemoglobin. When the blood moves through the body’s capillary system, the oxygen carried in the red blood cells is released from the iron to the other cells of the body.
White blood cells make up only about 1% pf the blood volume. They are an important part of the immune system. Their primary function is to provide defense against invaders in the body, which may include bacterial, parasites, fungi, and viruses. White blood cells may attack a foreign body directly, produce antibodies that identify, attach to and neutralize a foreign body, or they may trigger other cells to act in destroying the foreign body.
Platelets perform a vital function in the process of coagulation, or blood clotting, which occurs when a blood vessel is injured.
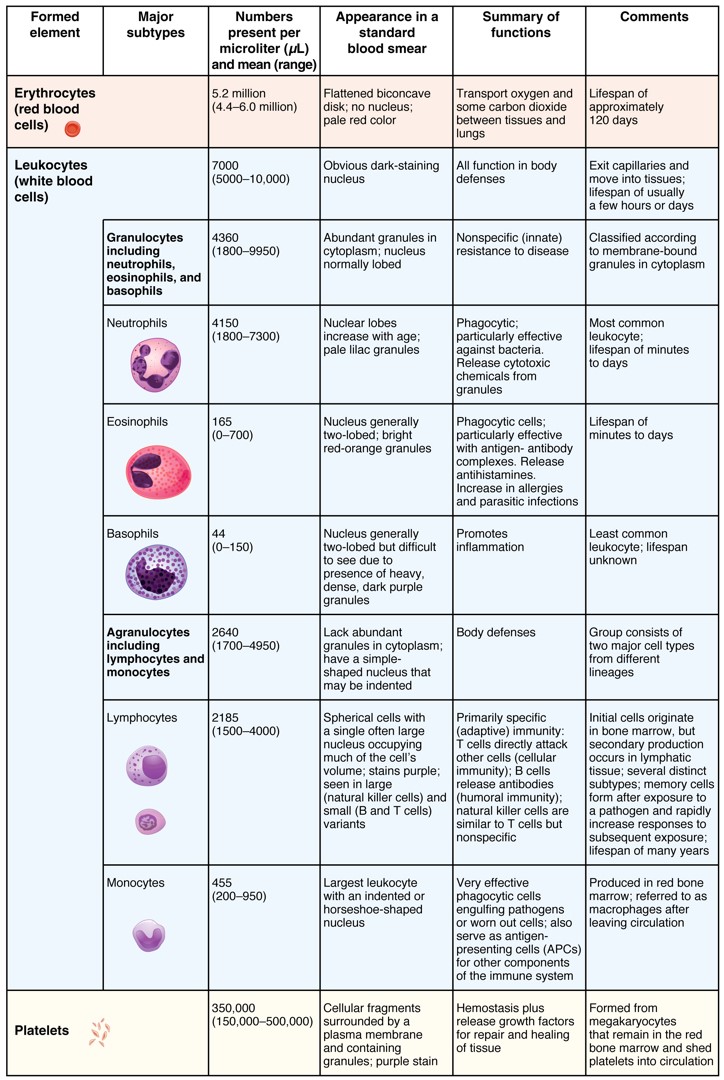
FORMED ELEMENTS
Erythrocytes (Red Blood Cells)
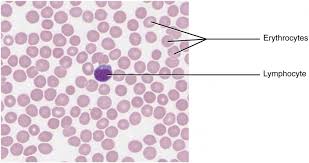
Erythrocytes are the cells that carry oxygen to tissues and waste products (like CO2) back to the lungs. They have a unique, biconcave-disk shape that is reminiscent of an old-timey cough drop: thin in the center, but thicker at the periphery. Erythrocytes have no nuclei and almost no organelles, but do contain large amounts of the oxygen-binding protein hemoglobin. Some estimates indicate there are as many as 300 million hemoglobin molecules per red blood cell. Erythrocytes are the most numerous formed elements.
Leukocytes (White Blood Cells)
Leukocytes are usually divided into two groups, based on the presence of granules that appear in the cytoplasm when stained: granular leukocytes (which contain granules), and agranular leukocytes (without granules). Leukocytes have immune functions.
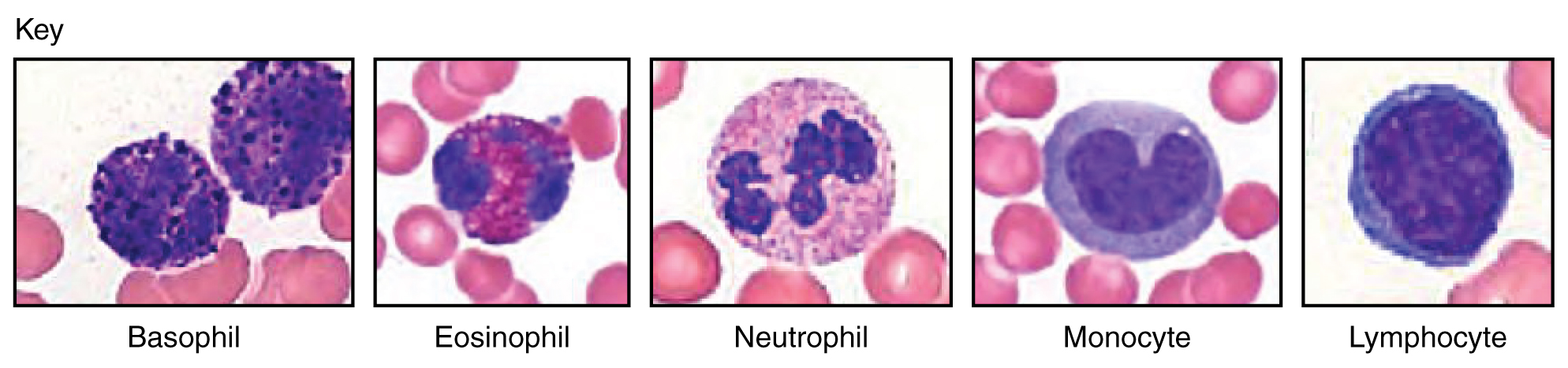
Agranular leukocytes: Lymphocytes
Lymphocytes are small cells that are notable for the large, darkly staining nucleus surrounded by a thin crescent of cytoplasm. These are the second-most numerous leukocytes.
Agranular leukocytes: Monocytes
Monocytes are large cells that have a large, horseshoe shaped or U-shaped nucleus. The surrounding cytoplasm tends to be light blue when stained.
Granular leukocytes: Neutrophils.
Neutrophils are so named because they do not interact strongly with a dye (hence, NEUTR-ophils). The cytoplasm may have a pink-ish or purplish tint and the granules may be pink or purple. They are notable for their multi-lobed nuclei in mature cells (although less-mature cells may have a horseshoe or U-shaped nuclei, making them difficult to distinguish from monocytes).Neutrophils are the most common leukocyte.
Granular leukocytes: Eosinophils
Eosinophils interact strongly with the acidic dye eosin, which stains the granules an orange color (and give them their name, EOSIN-ophils). The nuclei of eosinophils are lobed, like neutrophils, but the bright red-orange granules make these cells distinctive.
Granular leukocytes: Basophils
Basophils are small cells that interact strongly with basic dye (and so are named BAS-ophils), which stains the granules in the cytoplasm a dark blue color. The nuclei are often not visible through the dark granules. Basophils are the lease numerous leukocytes.
Platelets
Platelets are not cells, but rather cell fragments and thus are quite small. They have no organelles or nuclei, and they cytoplasm often stains purple or blue. They contain granules which may also stain dark blue or purple. Platelets play important roles in blood clotting.
Summary: Below is a table of the appearance and functions of the formed elements in the blood (Figure 18.7).
Blood Types and Blood Typing
In this exercise, you will determine the blood type of four different synthetic blood samples using antisera to the A, B, and Rh (D) antigens that exist on human red blood cells. The procedure for the blood test is the same that would be used for a real blood test, but for convenience and safety, the blood and antisera are synthetic and contain no biological materials.
Blood Types
Although the basic composition and function of blood in each of us is the same, there are different human blood types. The cell membrane of red blood cells, like that of other cells, has molecules that project from its surface. Some of the molecules function as identification badges, allowing the immune system to recognize the cell as normal component of an individual’s body. If blood from a person whose red cells have different surface molecules is injected into someone, those molecules are recognized as foreign to the body, or antigenic. The immune system attacks the antigens and attempts to destroy them and the cells that carry them. This is why transfusion with an incompatible blood type is harmful. The recipient’s body recognizes the antigens on the transfused red blood cells as foreign and attacks and destroys the cells. For that reason, donated blood is thoroughly tested for A, B, O and Rh antigens, and is transfused only into compatible recipients.
The ABO Blood Groups
The ABO blood groups (types) result from the presence or absence of two antigens, A and B, on the surface of the red blood cells. If antigens are present very early in life, the immune system recognizes those antigens as “self” and will not generate an immune response to them. As a result, the body does not generate antibodies to any A and B antigens present on its own blood cells. However, the immune system does produce antibodies to any A and B blood antigens not present on the organism’s own cells. Type A blood has the A antigen on its red blood cells and anti-B antibodies in the plasma. Type B blood has the B antigen on its red blood cells and A antibodies in the plasma. Type AB blood has both A and B antigens on the red blood cells and no antibodies in the plasma. Finally, type O blood has neither A nor B antigens on the red blood cells and both A and B antibodies in the plasma. These antibodies are present even if the person has not had any foreign blood introduced into their body. It is hypothesized that the antibodies are present because of similarity between the A and B blood antigens and other antigens present in the environment. If two antigens are similar enough, the antibodies generated to one antigen will also recognize the other.
The relationships of the ABO blood types to the presence of antigens and antibodies in the blood are summarized in the table that follows.
| Blood Group | Antigen Present on RBCs | Antibody Present in Plasma |
| A | A | Anti-B |
| B | B | Anti-A |
| AB | A and B | Neither anti-A nor anti-B |
| O | Neither A nor B | Both anti-A and anti-B |
The Rh Blood Groups
Another important antigen found on the surface of blood cells is the Rh factor. The Rh antigen is actually a whole group of closely related antigens. Blood containing an Rh antigen is said to be Rh positive (Rh+); blood lacking the antigen is said to be Rh negative (Rh-). Unlike the case for the ABO antigens, the production of Rh antibody requires prior exposure to the antigen, such as would occur in an Rh- pregnant woman carrying a fetus that was Rh+.
Pre-Laboratory Questions
After reviewing the background information, please answer the following questions.
1.Which of the following statements about blood is true?
Blood is about 92 percent water.
Blood is slightly more acidic than water.
Blood is slightly more viscous than water.
Blood is slightly more salty than seawater.
2.Which of the following statements about albumin is true?
It draws water out of the blood vessels and into the body’s tissues.
It is the most abundant plasma protein.
It is produced by specialized leukocytes called plasma cells.
All of the above are true.
3.Which of the following plasma proteins is not produced by the liver?
fibrinogen
alpha globulin
beta globulin
immunoglobulin
4. Why would it be incorrect to refer to the formed elements as cells?
5. True or False: The buffy coat is the portion of a blood sample that is made up of its proteins.
Exercises
- Exercise 1 Microscopy of formed elements on a prepared blood smear
- Exercise 2 Identifying the properties of formed elements (optional)
- Exercise 3 ABO-Rh blood typing with synthetic blood
- Exercise 4 Predicting the reactions of individual blood types with various anti-sera
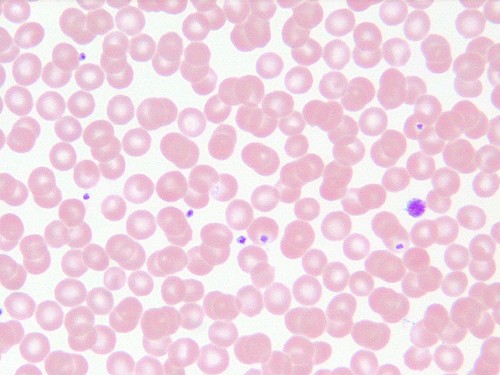
Exercise 1 Microscopy of formed elements on a prepared blood smear
Required Materials
- Compound microscope
- Microscope lens paper
- Microscope lens solution
- Microscope immersion oil
- Human Blood Wright’s smear
- Blood Cell Model
Procedure
- Ask your instructor for a prepared blood smear slide with Wright’s stain.
- Refer to the Figures 18.4, 18.5, 18.6 for what you expect to see.
- Place the slide on the stage of microscope and bring it into focus using low power (4 x 10 magnification).
- Change the magnification to high power (10 x 10), followed by 40 x 10. Focus. Flip objective so that the slide is between the 40x and 100x objective.
- Add a drop of immersion oil onto the coverslip.
- Click the 100x objective onto the drop of oil. Use the fine focus adjustment to focus.
- Draw the formed elements at this 100 x 10 magnification.
- Identify the following formed elements based on the illustrations provided in the table. Note that some elements will be much easier to locate than others due to their relative abundance in whole blood: Basophils, Eosinophils, Erythrocytes, Lymphocytes, Monocytes, Neutrophils and Platelets.
- Sketch and label each formed element you observe in the space below.

Exercise 2 Identifying the properties of formed elements (optional)
Using the data collected from the microscopic observation of prepared human blood smear slide and included tabulated information on formed elements, complete the following table of information on formed elements of blood.
| Formed Element | Nucleus Shape or Appearance | Other Features of the Cytoplasm / Granules | Functions |
| Erythrocyte
|
|||
| Basophil
|
|||
| Eosinophil
|
|||
| Lymphocyte
|
|||
| Monocyte
|
|||
| Neutrophil
|
Exercise 3 ABO-Rh blood typing with synthetic blood
Required Materials
- Understanding Blood Type Interactions Kit (Aldon IS3103)
- Simulated blood samples (4), in dropper vials
- Simulated anti-A, anti-B, and anti-Rh serum, in dropper vials
- Plastic well plates for blood typing
- Plastic toothpicks for stirring
Procedure
- Using the dropper vial, place a drop of Sample 1 in each well of the blood typing well plate.
- To prevent contamination, always close the cap on one vial before opening the next vial.
- Add a drop of anti-A serum to well A. Close the cap.
- Add a drop of anti-B serum to well B. Close the cap.
- Add a drop of anti-Rh serum (anti-D) to well Rh. Close the cap.
- Using a different mixing stick for each well, gently stir the synthetic blood and antiserum drops for 30 seconds. Remember to use a new mixing stick for each sample to avoid contamination of our samples. Carefully examine the resulting thin films of liquid in each well. If a film is uniform in appearance there is no agglutination. If the sample appears granular, agglutination has occurred.
- Enter your results in the following data table. Enter YES if agglutination has occurred, NO if there is no agglutination. Get a clean slide and repeat the above steps for samples 2 – 4.
Data Table – Results of mixing synthetic blood samples with various anti-serums.
| Sample 1 | Sample 2 | Sample 3 | Sample 4 | |
| Anti-A serum
|
||||
| Anti-B serum
|
||||
| Anti-Rh serum
|
||||
| Blood type?
|
Exercise 4 Predicting the reactions of individual blood types with various anti-sera
Fill in the table with predictions. Indicate whether you expect to see agglutination (“clumping”) or no agglutination when each of the following blood types is mixed with each anti-serum. (Anti-serum contains antibodies, so anti-A antiserum contains anti-A antibodies, anti-B antiserum contains anti-B antibodies, and anti-Rh serum contains anti-Rh antibodies)
Data Table – Predicted reactions when different blood types are mixed with various anti-sera.
| Blood type | When mixed with anti-A serum…. | When mixed with anti-B serum… | When mixed with anti-Rh serum… |
| A+
|
|||
| A –
|
|||
| B+
|
|||
| B-
|
|||
| AB+
|
|||
| AB-
|
|||
| O+
|
|||
| O-
|
Post-laboratory Questions
1. Which of the following statements about mature, circulating erythrocytes is true?
a. They have no nucleus.
b. They are packed with mitochondria.
c. They survive for an average of 4 days.
d. All of the above
2. The production of healthy erythrocytes depends upon the availability of ________.
a. copper
b. zinc
c. vitamin B12
d. copper, zinc, and vitamin B12
3. Which of the following describes a neutrophil?
a. abundant, agranular, especially effective against cancer cells
b. abundant, granular, especially effective against bacteria
c. rare, agranular, releases antimicrobial defensins
d. rare, granular, contains multiple granules packed with histamine
4. A patient has been experiencing severe, persistent allergy symptoms that are reduced when she takes an antihistamine. Before the treatment, this patient was likely to have had increased activity of which leukocyte?
a. basophils
b. neutrophils
c. monocytes
d. natural killer cells
5. Thrombocytes are more accurately called ________.
a. clotting factors
b. megakaryoblasts
c. megakaryocytes
d. platelets
6. The process by which leukocytes squeeze through adjacent cells in a blood vessel wall is called ________.
a. leukocytosis
b. positive chemotaxis
c. emigration
d. cytoplasmic extending
7. The process in which antibodies attach to antigens, causing the formation of masses of linked cells, is called ________.
a. sensitization
b. coagulation
c. agglutination
d. hemolysis
8. People with ABO blood type O ________.
a. have both antigens A and B on their erythrocytes
b. lack both antigens A and B on their erythrocytes
c. have neither anti-A nor anti-B antibodies circulating in their blood plasma
d. are considered universal recipients
9. Hemolytic disease of the newborn is a risk during a subsequent pregnancy in which ________.
a. a type AB mother is carrying a type O fetus
b. a type O mother is carrying a type AB fetus
c. an Rh+ mother is carrying an Rh− fetus
d. an Rh− mother is carrying a second Rh+ fetus
10. Hemophilia is characterized by ________.
a. inadequate production of heparin
b. inadequate production of clotting factors
c. excessive production of fibrinogen
d. excessive production of platelets

