20 Chapter 20 The Cardiovascular System: Blood Vessels and Circulation
By Aylin Marz
Motivation.
Sars-Cov-2 virus causing the COVID-19 pandemic affects many systems of the body including those related to circulation. Blood clots, injured blood vessels, and bleeding found in lungs and effects on the heart as well as other body parts have been found in autopsies of patients who died from COVID-19. Since all organs use blood vessels the clots that block blood flow or injuries to blood vessels may explain how this unusual virus causes multi-organ damage, unlike many other viruses that have specific targets.
Learning Objectives
Upon completion of the work in this chapter students should be able to:
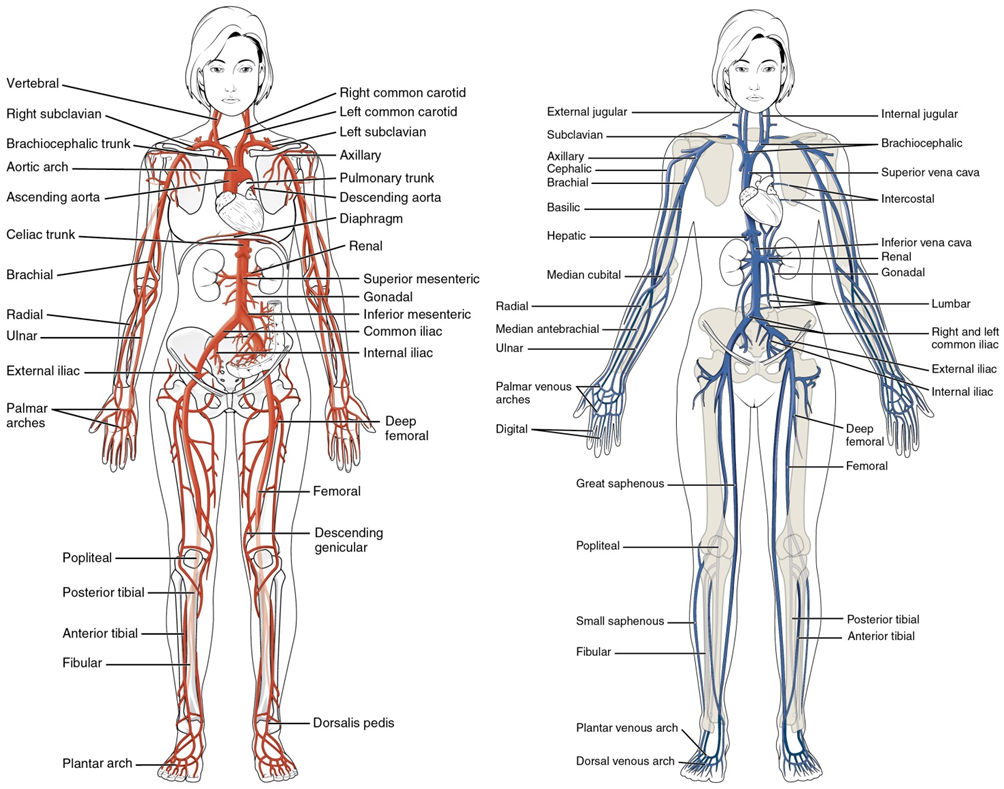
- Identify the major arteries and veins of the body using a torso model
- Perform arterial blood pressure measurement utilizing a pressure cuff and stethoscope
- Analyze factors that affect blood flow and blood pressure.
Background.
Structure and Function of Blood Vessels
Blood pumped by the heart flows through a series of vessels known as arteries, arterioles, capillaries, venules, and veins before returning to the heart (Figure 20.2). Arteries transport blood away from the heart and branch into smaller vessels, forming arterioles. Arterioles distribute blood to capillary beds, the sites of exchange with the body tissues. Capillaries lead back to small vessels known as venules that flow into the larger veins and eventually back to the heart.
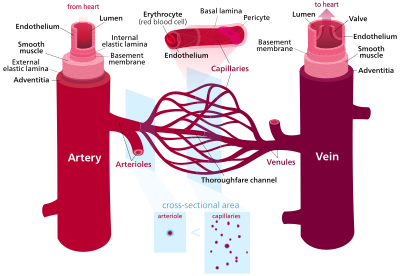
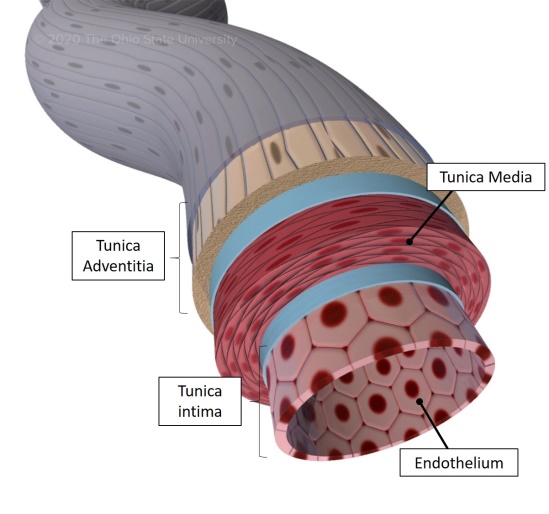
The arterial system is a relatively high-pressure system, so arteries have thick walls that appear round in cross section (Figure 20.3). The venous system is a lower-pressure system, containing veins that have larger lumens and thinner walls. They often appear flattened. Arteries, arterioles, venules, and veins are composed of three tunics known as the tunica intima, tunica media, and tunica externa. Capillaries have only a tunica intima layer. The tunica intima is a thin layer composed of a simple squamous epithelium known as endothelium and a small amount of connective tissue. The tunica media is a thicker area composed of variable amounts of smooth muscle and connective tissue. It is the thickest layer in all but the largest arteries. The tunica externa is primarily a layer of connective tissue, although in veins, it also contains some smooth muscle. Blood flow through vessels can be dramatically influenced by vasoconstriction and vasodilation in their walls.
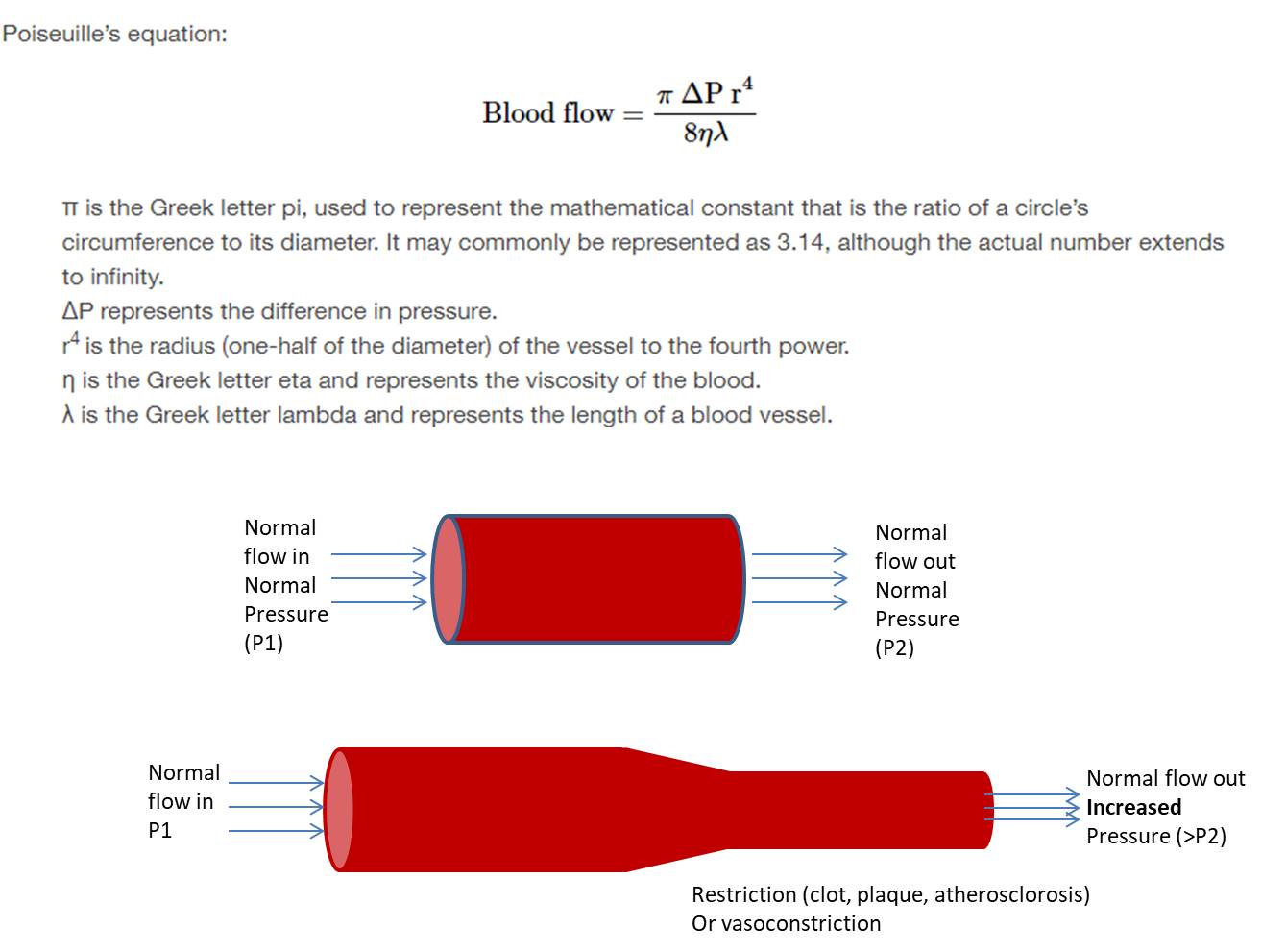
Blood Flow, Blood Pressure and Resistance
Blood flow is the movement of blood through a vessel, tissue, or organ. The slowing or blocking of blood flow is called resistance. Blood pressure is the force that blood exerts upon the walls of the blood vessels or chambers of the heart. The components of blood pressure include systolic pressure, which results from ventricular contraction (of the heart), and diastolic pressure, which results from ventricular relaxation. Pulse pressure is the difference between systolic and diastolic measures, and mean arterial pressure is the “average” pressure of blood in the arterial system, driving blood into the tissues. Pulse, the expansion and recoiling of an artery, reflects the heartbeat. The variables affecting blood flow and blood pressure in the systemic circulation are cardiac output (amount of blood pumped by heart per minute), compliance, blood volume, blood viscosity, and the length and diameter of the blood vessels.
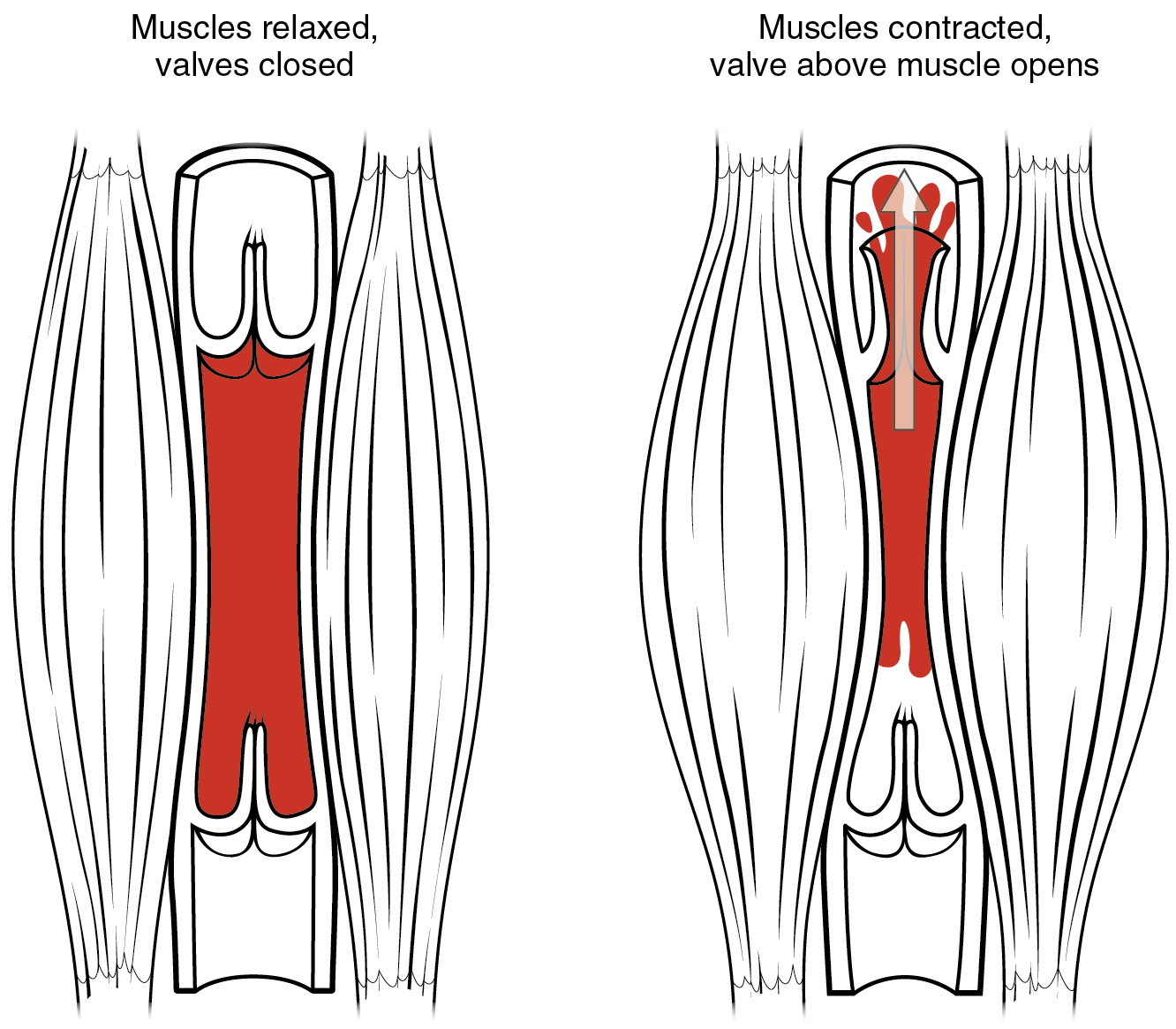
In the arterial system, vasodilation and vasoconstriction of the arterioles is a significant factor in systemic blood pressure: Slight vasodilation greatly decreases resistance and increases flow, whereas slight vasoconstriction greatly increases resistance and decreases flow. In the arterial system, as resistance increases, blood pressure increases and flow decreases. In the venous system, constriction increases blood pressure as it does in arteries; the increasing pressure helps to return blood to the heart. In addition, constriction causes the vessel lumen to become more rounded, decreasing resistance and increasing blood flow. Venoconstriction, while less important than arterial vasoconstriction, works with the skeletal muscle pump, the respiratory pump, and their valves to promote venous return to the heart (Figure 20.4).
Capillary Exchange
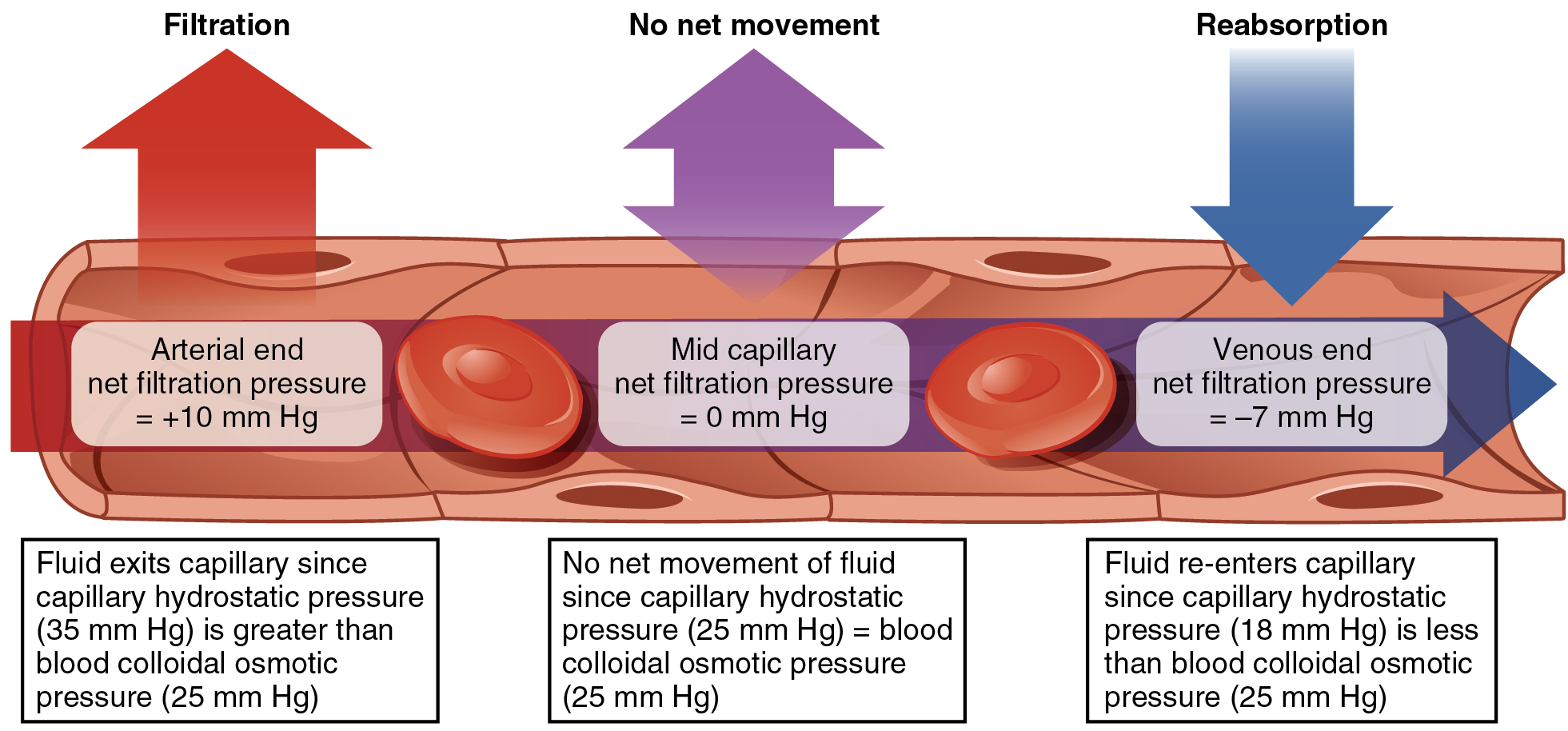
Small molecules can cross into and out of capillaries via simple or facilitated diffusion. Some large molecules can cross in vesicles or through clefts, fenestrations, or gaps between cells in capillary walls. However, the bulk flow of capillary and tissue fluid occurs via filtration and reabsorption. Filtration, the movement of fluid out of the capillaries, is driven by the capillary hydrostatic pressure or CHP. Reabsorption, the influx of tissue fluid into the capillaries, is driven by the blood colloid osmotic pressure or BCOP. Filtration predominates in the arterial end of the capillary; in the middle section, the opposing pressures are virtually identical so there is no net exchange, whereas reabsorption predominates at the venule end of the capillary. The hydrostatic and colloid osmotic pressures in the interstitial fluid are negligible in healthy circumstances (Figure 20.5).
Homeostatic Regulation of the Vascular System
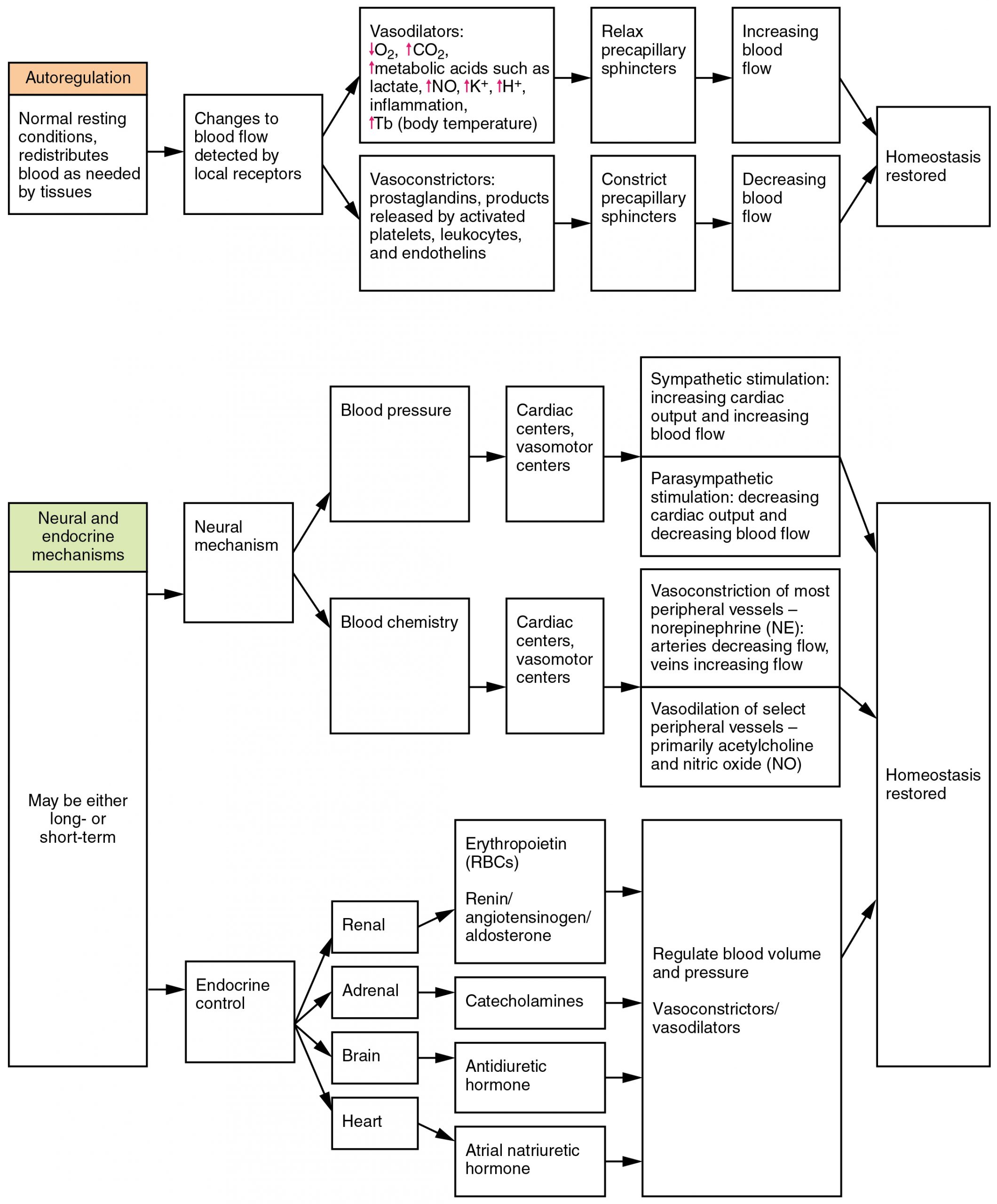
Neural, endocrine, and autoregulatory mechanisms affect blood flow, blood pressure, and eventually perfusion of blood to body tissues (Figure 20.6). Neural mechanisms include the cardiovascular centers in the medulla oblongata, baroreceptors in the aorta and carotid arteries and right atrium, and associated chemoreceptors that monitor blood levels of oxygen, carbon dioxide, and hydrogen ions. Endocrine controls include epinephrine and norepinephrine, as well as antidiuretic hormone ADH, the renin-angiotensin-aldosterone mechanism, atrial natriuretic hormone ANH, and erythropoietin EPO. Autoregulation is the local control of vasodilation and constriction by chemical signals and the myogenic response (response of smooth muscles of the blood vessels). Exercise greatly improves cardiovascular function and reduces the risk of cardiovascular diseases, including hypertension, a leading cause of heart attacks and strokes. Significant hemorrhage can lead to a form of circulatory shock known as hypovolemic shock. Sepsis, obstruction, and widespread inflammation can also cause circulatory shock.
Circulatory Pathways
The right ventricle pumps oxygen-depleted blood into the pulmonary trunk and right and left pulmonary arteries, which carry it to the right and left lungs for gas exchange. Oxygen-rich blood is transported by pulmonary veins to the left atrium. The left ventricle pumps this blood into the aorta (Figure 20.7).
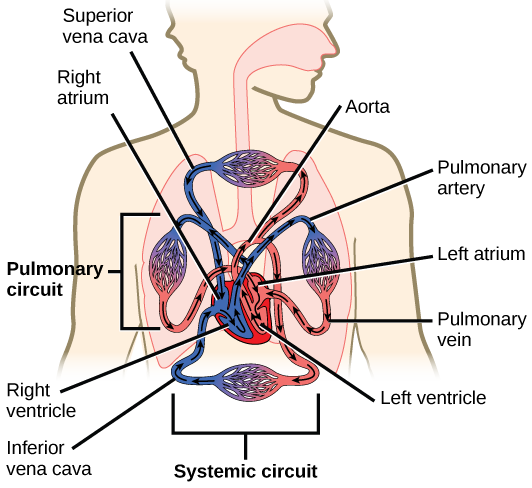
The main regions of the aorta are the ascending aorta, aortic arch, and descending aorta, which is further divided into the thoracic and abdominal aorta. The coronary arteries that oxygenate the heart itself branch from the ascending aorta. After oxygenating tissues in the capillaries, systemic blood is returned to the right atrium from the venous system via the superior vena cava, which drains most of the veins superior to the diaphragm, the inferior vena cava, which drains most of the veins inferior to the diaphragm, and the coronary veins via the coronary sinus. The hepatic portal system carries blood to the liver for processing before it enters circulation.
Pre-Laboratory Questions
After you review the Background information above, answer the following questions before attempting the Exercises in the laboratory.
- Name one structural feature of arteries that help their function.
- What is the function of valves in veins?
- How does having just a tunica interna and no other layers help the function of capillaries?
- Define the terms vasoconstriction and vasodilation.
- List the main arteries and veins blood follows as it is pumped from the heart to the lungs and back in the pulmonary circuit.
- List the main arteries and veins blood follows as it travels from the heart to the rest of the body and back to the heart again.
Exercises
- Exercise 1 Examine the microanatomy of blood vessels (optional)
- Exercise 2 Identify the main arteries and veins of the body on a torso model
- Exercise 3 Measure blood pressure using a blood pressure cuff and stethoscope
- Exercise 4 Analyze factors affecting blood pressure
Exercise 1 Examine the microanatomy of blood vessels (optional)
Required Materials
- Compound microscope
- Microscope lens paper
- Microscope lens solution
- Microscope immersion oil
- Human Artery and Vein prepared microscope slide
Procedures
- Obtain a microscope and plug it in on your bench. Make sure the objective and ocular lenses are clean. If not, use the lens paper and lens cleaning solution to wipe these.
- Turn on the microscope and adjust the ocular lens distance until you see only one lit circle when you look through the eyepiece.
- Obtain a human artery and vein slide and first observe it using the 4x objective to focus, 10x and 40x to see higher magnification. Compare your observations with the blood vessel structure drawings in figures 20.2 and 20.3 to better understand what you are seeing.
- Sketch and label what you observe using low magnification and high magnification in the space below. Your sketch should allow you to label the following structures: artery, vein, capillary, endothelium, tunica interna, tunica media (on vein and artery only), tunica externa (on vein and artery only), and valve (if present, on vein only).
Exercise 2 Identify the main arteries and veins of the body on a torso model
Required Materials
- Torso model
- Circulatory system model
- Post-it notes
- Labeling tape
Procedures
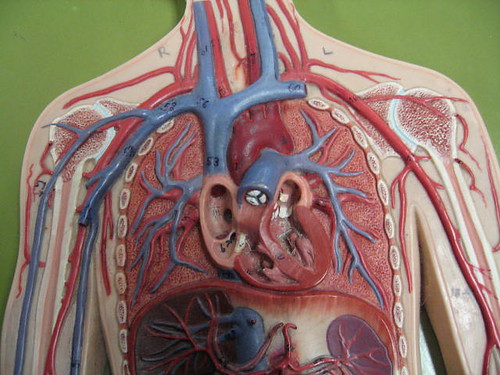
- You will find multiple torso models that also contain arteries and veins as part of them, similar to the image shown in Figure 20.9. Select a torso model and remove the plastic organs to expose the blood vessels.
- Use the post-its or the labeling tape to name the main arteries and veins. Refer to Figure 20.8 showing the main arteries and veins of the human body to check your work and for guidance.
- Take a picture with your labeled blood vessels on the model and paste in the space below. Alternatively, you can sketch the model with blood vessels and label it in the space below.

Exercise 3 Measure blood pressure using a blood pressure cuff and stethoscope
Required Materials
- Syphygmomanometer (blood pressure cuff)
- Stethoscope
Procedure
In this exercise you will learn to measure blood pressure and test the effects of exercise on blood pressure.
Follow the steps below to measure the resting systolic and diastolic blood pressure. Record the values here:
-
- Resting Systolic Pressure:___________
- Resting Diastolic Pressure: __________
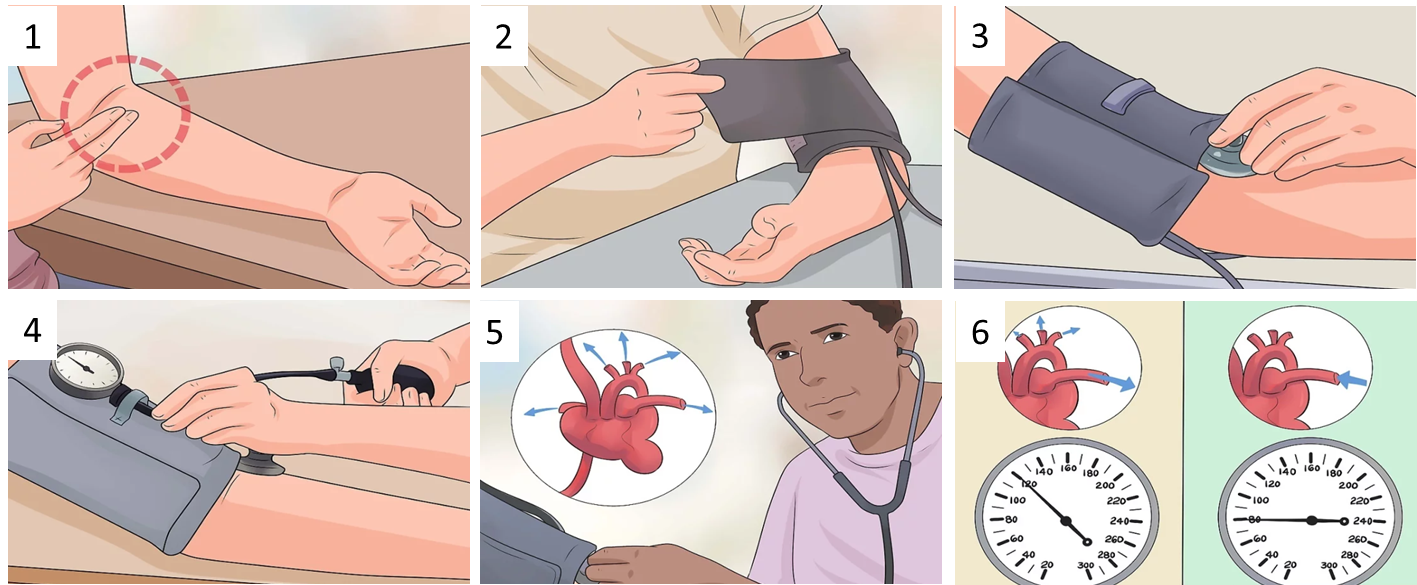
1.Locate the pulse. Place your index and middle fingers over the inside center of the inner elbow. When you press lightly you should be able to feel the pulse of the brachial artery from this position. If you have difficultly locating your pulse, place the head of the stethoscope (the round piece at the end of the tube) in the same general area and listen until you can hear the heartbeat.
2.Wrap the cuff around the arm and tighten. Tuck the cuff end through the metal loop and slide it onto your upper arm. The cuff should be roughly 1 inch (2.5 cm) above the bend of your elbow and should be evenly tight around your arm. Make sure that the skin is not pinched by the cuff as you wrap it securely. The cuff should have heavy duty velcro on it, which will hold the cuff closed.
3.Place the stethoscope under the cuff. The head should be face down, with the wide part of the chest piece in contact with the skin. It should be positioned directly over the pulse of your brachial artery that you found earlier. Also place the stethoscope earpieces in your ears. The earpieces should face forward and point toward the tip of your nose.
4.Inflate the cuff until no blood flow sounds are heard with stethoscope. The gauge needs to be positioned where you can see it. You should hold the pump in your right hand.Turn the screw on the pump bulb clockwise to close the airflow valve, if necessary. Rapidly squeeze the pump bulb until you no longer hear the sound of the pulse through the stethoscope. Stop once the gauge reads 30 to 40 mmHg above normal blood pressure, usually between 160 to 180 mmHg.
5.Deflate the cuff slowly and listen for systolic reading. Open the airflow valve by twisting the screw counterclockwise. Let the cuff deflate gradually.The gauge should fall 2 mm, or two lines on the gauge, per second. Note the measurement on your gauge at the precise moment you hear ythe heartbeat again. This measurement is your systolic reading. Systolic blood pressure refers to the force your blood exerts against the artery walls as your heart pumps. This is the blood pressure created when your heart contracts.
6.Continue deflating the cuff and listen for diastolic reading. Note the measurement on your gauge at the precise moment the sound of the heartbeat disappears. This measurement is your diastolic reading. Diastolic blood pressure refers to your blood pressure in between heartbeats.
For an adult, the systolic blood pressure should be less than 120 mmHg and the diastolic blood pressure should be less than 80 mmHg. This range is considered “normal.”
Exercise 4 Analyze factors affecting blood pressure
In this exercise we will determine the effect of hot and cold water immersion on blood pressure and blood flow.
Remember that sufficient blood flow is necessary for organ function. However, too much blood abnormally diverted to an area can challenge the integrity of the blood vessels increasing risk of rupture. As our nervous, endocrine and local control mechanisms respond to changes like exercise and cold, the radius/diameter of some blood vessels is changed; vasoconstricting to reduce blood flow and vasodilating to increase blood flow. Vasoconstriction and vasodilation in turn affect blood pressure (Figure 20.11).
Required Materials
- Syphygmomanometer (blood pressure cuff)
- Stethoscope
- Ice bath (ice, in large beaker or bucket)
- Warm water bath (hot plate, large beaker or bucket)
- Thermometer
Procedures
1.Follow the steps described in Exercise 3 (Figure 20.10) above to measure blood pressure of a classmate (subject) who is resting, and record it:
-
- Resting Systolic Pressure:________
- Resting Diastolic Pressure: __________
2.Prepare an ice bath in a large beaker (or other container) placing sufficient ice to bring down the water temperature to 0-10oC.
3.Ask your classmate (subject) to immerse their left hand in the ice bath for 5 minutes.
4.While the hand is still in the ice bath, measure blood pressure and record it:
-
- Cold Systolic Pressure:________
- Cold Diastolic Pressure: __________
5.Remove your classmate’s hand from ice water and let them rest while you prepare a warm water bath. Warm up the water on a hotplate but make sure you do not exceed 40oC. You can mix warm and tapwater to obtain the temperature needed.
6.Have your classmate immerse their hand in the warm water container for 5 minutes.
7.While the hand is still in the ice bath, measure blood pressure and record it.
-
- Warm Systolic Pressure:________
- Warm Diastolic Pressure: __________
Post-laboratory Questions
1.In Exercise 1, you observed normal capillary, artery and vein structure. Below you have a diseased artery in the kidney (Figure 20.12).
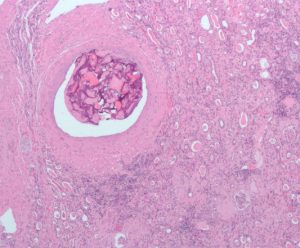
Compare and contrast the structure of this artery with the normal artery you observed.
-
- List the similarities between this diseased artery and the normal artery features you observed.
- List what is different in this artery compared to the normal artery you observed.
- What effect would you expect this artery problem to have on blood flow? Blood pressure? Explain.
2.In Exercise 3, did blood pressure increase or decrease after cold treatment? Why do you think this change occurred? Explain.
3.In Exercise 3, did blood pressure increase or decrease after warm treatment? Why do you thin this change occurred? Explain.